Examining a Patient with Suspected Stroke
Essentially the NIH Stroke Scale is the most targeted, well validated and universally adopted way to examine in suspected AIS.
It takes a bit of practice to become efficient!
The NIHSS is a 15-item neurologic examination stroke scale used to evaluate the effect of acute cerebral infarction on the levels of consciousness, language, neglect, visual-field loss, extraocular movement, motor strength, ataxia, dysarthria, and sensory loss.
A trained observer rates the patient’s ability to answer questions and perform activities. Ratings for each item are scored on a 3- to 5-point scale, with 0 as normal, and there is an allowance for untestable items. Scores range from 0 to 42, with higher scores indicating greater severity.
A single patient assessment requires less than 10 minutes to complete.
The evaluation of stroke severity depends upon the ability of the observer to accurately and consistently assess the patient.
Stroke severity may be stratified on the basis of NIHSS scores as follows:
Very Severe: >25
Severe: 15 – 24
Mild to Moderately Severe: 5 – 14
Mild: 1 – 5
How do you do the NIHSS?
NIHSS Calculator
Here’s an online calculator
VISUAL AIDS
To help you remember it at the bedside!

Our patient, Jose, has the following findings:
Alert and oriented
Left-sided visual inattention
Left-sided complete homonymous hemianopia
Smile asymmetry on left side of face
Left arm no effort against gravity
Left leg no movement
Right arm and leg normal
No ataxia
Mild sensory loss on left side – less sharp, more dull
Dysarthria, slurring but can be understood
> What is his NIHSS?
Stroke Syndromes
Reality is never as clean as these descriptions imply, so don’t get too caught up on this.
LEFT
Right hemiplegia of arms and face (motor + premotor cortex)
Right hemisensory loss of arms and face (somatosensory cortex)
Aphasia (Broca’s area, pars opercularis)
Gaze deviation towards left (frontal eye field)
Right homonymous hemianopia (optic radiation)
Superior division
- motor cortex
- Superior visual radiation
- Broca’s area
Inferior division
- Wernickes area
- Inferior visual radiation
RIGHT
Left hemiplegia of arms and face
Left hemisensory loss of arms and face
Left sided neglect (parietal region)
Gaze deviation to the right
Left-sided homonymous hemianopia
Contralateral leg weakness
Contralateral sensory loss of legs
Cognitive changes e.g. abulia
If recurrent artery of Huebner
- Contralateral hemiparesis (internal capsule)
- Movement disorder (caudate head)
Anterior Choroidal Artery
Contralateral visual field defects (lateral geniculate nucleus)
Contralateral hemiparesis (internal capsule)
Contralateral hemisensory loss (internal capsule)
Contralateral homonymous hemianopia (occipital lobe)
Impaired short-term memory (medial temporal/ hippocampus)
Alexia without agraphia (left inferior temporal lobe)
Prosopagnosia (right inferior temporal lobe)
Changes in level of arousal (thalamus)
If artery of Percheron affected:
- Left and right thalami supplied by single artery from PCA
- Altered mental status
Corticospinal – limb weakness, often bilateral, limb hyperreflexia, extensor plantar response
Corticobulbar- facial weakness, dysarthria, dysphagia, increased gag reflex
Oculomotor – diplopia, gaze palsies, nystagmus, INO
Reticular activating system- reduced consciousness
Lateral pontine syndrome
Vertigo, vomiting, nystagmus (vestibular nuclei)
Ipsilateral loss of sensation in face (principal sensory trigeminal nucleus)
Facial paralysis (facial nucleus)
Hearing loss, tinnitus (cochlear nucleus)
Lateral medullary syndrome
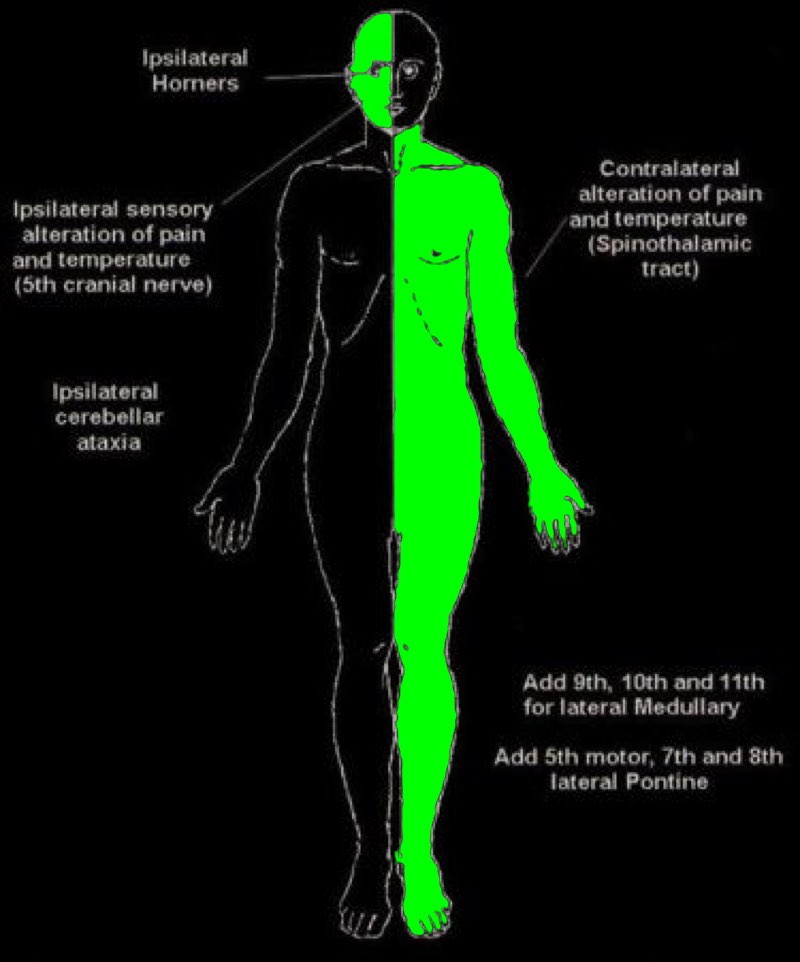
Contralateral loss of pain and sensation in body (spinothalamic tract)
Ipsilateral facial loss of pain and temperature (spinal trigeminal nucleus)
Dysphasia, dysphonia (nucleus ambiguous)
Vertigo, diplopia, nystagmus, vomiting (inferior vestibular nucleus)
Ipsilateral Horners (sympathetic fibers)
Palatal clonus (central trigeminal tract)
Ataxia (inferior cerebellar peduncle)
Occlusion of small penetrating arteries affecting subcortical matter
Pure motor
- Posterior limb of internal capsule or anterior pons
Pure sensory
- VPL / VPM nuclei of thalamus
Ataxia + hemiparesis
- corticospinal tract + corticopontocerebellar fibres
- Either at internal capsule or anterior pons
Dysarthria + clumsy hand
- Internal capsule or anterior pons