Resus Priorities
Although these are listed here, you will obviously be doing much of this concurrently.
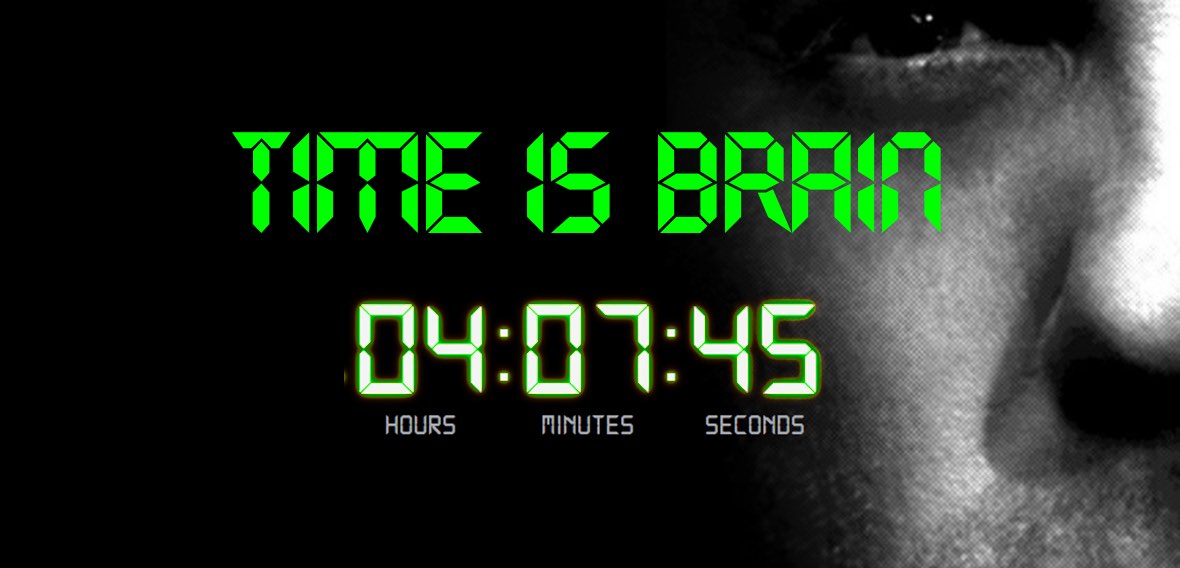
> Remember TIME IS BRAIN. Refer immediately, activate local stroke protocol as soon as stroke suspected
> Aim oxygen sats > 94%.
> Get IV access, preferably with 18G IVC
> Treat hypertension if SBP > 185 or DBP > 110 mmHg to maintain thrombolysis eligibility> Get a good history, specifically thinking of time when “last known well” and of factors that rule in or out thrombolysis and ECR including medications.
> Exam centres around NIHSS
> Bloods (looking for thrombolysis exclusions) and imaging: CT, CTA, CTP
> Don’t miss treatable stroke mimics
> Get to a stroke centre ASAP if potentially suitable
> Keep nil by mouth
WHY RARELY AN ISSUE?
Most patients who’ve had strokes do not require intubation.
Usually minimal oxygen is required for a target oxygen saturation > 94%
The location of the stroke is probably the most relevant factor related to the need for mechanical ventilation, rather than the particular type of cerebrovascular pathology.
In this context, impairment of the following brain areas increases the risk of respiratory failure:
> Level of consciousness:
Thalami, the limbic system, the reticular formation in the brainstem
> Breathing:
Respiratory centres in the cortex, pons, and medulla
> Swallowing:
Medulla and brainstem connections
WHEN TO INTUBATE?
If it aligns with the patient’s known wishes and:
> Reduced level of consciousness with threatened airway (e.g. concomitant brain injury, shock, medications given etc)
> Respiratory depression causing hypercapnia or hypoxia
> Suspicion of aspiration pneumonitis causing hypoxia
TIPS FOR INTUBATION
> Maintain oxygenation, avoid hypotension and avoid further neuronal damage
> Do a neurological assessment including a NIHSS before giving sedation
> Use only short acting sedative / analgesic agents
> Haemodynamic instability is rare.
> Exisiting hypertension is common
> Initial BP targets are broad:
100-180 mmHg non-invasive systolic blood pressure
Age
Time last seen well (or time of onset if known)
Stroke symptoms
Baseline Modified Rankin Scale
– Scale of neurologic disability from 0 (completely normal) – 6 (dead)
– MRS </= 2 (i.e. independent with ADLs) are eligible for ECR
Past medical history (specifically factors that would preclude TPA)
– Stroke, head trauma, neurosurgery in past 3 months
– History of intracranial haemorrhage
– Known intracranial AVM, aneurysm or neoplasm
– Active internal bleeding
– Suspected/ confirmed endocarditis
– Known bleeding diathesis
– Recent GIT or urinary tract haemorrhage last 21 days (relative contraindication)
– Major surgery or serious non-head trauma last 14 days (relative contraindication)
Medications
> Anticoagulation: NOACS, warfarin, aspirin, clopidogrel, time meds last taken
> Vital signs
Uncontrolled hypertension SBP >185 mmHg or DBP >110 mmHg is contraindication to TPA
> GCS
> NIHSS (see next topic)
Click on the differentials below to see how to rule them out…
Early investigations
> Blood glucose
> Bloods:
Platelets (<100 a CI)
aPTT
INR (> 1.7 a CI)
Beta HCG (pregnancy a CI)
CT Brain:
> Non contrast
> CT angiogram arch to COW
> CT Perfusion
> Look for arrhythmias especially atrial fibrillation
Also look for evidence of:
Ischaemia
Heart failure
QT prolongation
Heart block
Paced rhythm
Next steps
Remember, time is brain.
Refer early before you have all the info.
> Airway status
> Last known well (LKW) time
> NIHSS
> Coagulation parameters—PT, PTT, INR
> CT—dense MCA sign, MCA dot sign, dense basilar sign, ASPECTS score if given, early ischemic changes
> CTA/MRA—large vessel occlusion (ICA, M1, M2, basilar, PCA)
> CTP—volume of core and penumbra, matched or mismatched perfusion
> Thrombolytic administration—yes (initiation, completion time); no (reason)
> Endovascular intervention (time to groin puncture, recanalization, TICI score)
> Target BP
18G IVC in good vein
> Will need CTA and potentially thrombolysis via this
> New lines riskier post thrombolysis
Keep NBM until swallow formally assessed
> Follow local institutional guidelines
