What is End of Life Care?
> Patient centred care focusing on quality of life: managing symptoms, providing comfort and assistance
> Used when there is medical consensus that there is an irreversible life threatening disease process
> Includes help with emotional and mental health needs of a patient and their family
> Essentially the same as Palliative Care
There’s only one chance to get it right
A Good Death
This depends on the views of an individual but patient priorities include:
- Freedom from pain and other uncomfortable symptoms
- Avoiding inappropriate prolongation of dying
- Relieving burden on others
- A degree of control, autonomy and independence
- Respect of their wishes including appropriate limitations of use of aggressive treatments
The Practicalities
Patients for whom there is medical consensus that they have an irreversible life-threatening condition.
It is an inclusive and collaborative decision involving the patients family.
All of the neurological emergencies in this course may end in this way.
If there is sufficient uncertainty about prognosis, or if there is disagreement between treating specialists about prognosis, usual practice is for more time to be given.
When prognosis is uncertain and therapies entail suffering, the pros and cons of each therapy must be weighed up with the patient’s wishes and experience in mind.
When it becomes clear that a condition is irreversible and the family are prepared for the change in focus of care.
This entails all the required investigations to confidently reach this conclusion, conversations with the involved specialist teams and a conversation with the family.
Always think of organ donation when a ventilated patient is dying in ICU
> Care of a dying patient and their family involves respecting their views on organ and tissue donation
> Notify a Organ Donation Specialist Nurse to discuss suitability as soon as they are identified as for end-of-life care
> The next section covers this in more detail
Who should attend the Family Meeting?
Senior treating Doctor
Nursing caring for Patient
Social Worker
+/- Donation Specialist Nurse
An Approach
> Engage and empathise with family
> Explore how they are
> Give space for them to talk
> Be open, honest and compassionate
> Check what they understand already
> Recap events in simple terms that won’t confuse or overwhelm with information
> Involve other teams if the are available
> Use the word “die” rather than ambiguous euphemisms
> Give time for this to register
> If organ donation is a possibility, ideally separate that discussion to avoid overwhelming the family
Here’s an example:
Withholding and Withdrawing
Care is never withheld or withdrawn.
> This is important. Good end-of-life care is every bit as important as many treatments we offer.
> Care is never withdrawn or withheld
> Non-beneficial treatments often are.
When patients describe a “good death” they say they want to avoid prolongation of dying REF
In Australia, NZ, the UK and the USA there is agreement that where treatment is not going to succeed (deemed “non-beneficial”), it should be withheld or withdrawn REF
There is a wide variation in practices around withholding and withdrawing treatment across countries.
Australian Law
This information comes from an excellent resource authored by Professors Ben White and Lindy Willmott and Penny Neller. REF
> When is it lawful to withhold or withdraw futile or non-beneficial treatment?
Once it is discussed with the family that the focus is now End-of-life care, performing CPR and ALS when they die is obviously not appropriate.
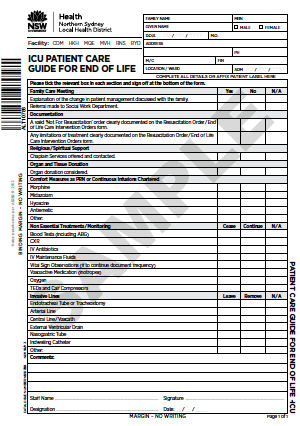
The order “Not for resuscitation” should be documented.
The principle
To provide sufficient analgesia so the patient is not suffering
The Law
The doctrine of double effect has been adopted by the common law in end of life treatment.
It is the ethical and legal justification for using medications such as opioids in end-of-life care, when the intent that they are being used is primarily to relieve pain and suffering, even if an unintended consequence is shortening a patient’s life. REF
This principle distinguishes euthanasia from palliative care based on the intentions of the physician’s use of the medication.
Key elements which must be met to be within the law are:
> The intent of the prescribed medications must be to relieve pain rather than kill
> Context specific: only applies if a patient is near death
> The medications and doses used should be considered “good medical practice”
An Approach
Prescribe opiates to be titrated to specific physiological parameters that represent pain or distress:
> Respiratory rate < 20 breaths per minute
> Heart rate < 100 bpm
The amount of opiate required will depend on:
- The degree of pain or discomfort
- The patients age, sex and weight and organ function
- Their existing tolerance of opiates
Typical adult dosing may be:
2-10 mg IV morphine
Followed by IV morphine infusion 0.05–0.5 mg/kg/h
Fentanyl or oxycodone are accepted alternatives
In the context of renal failure:
Hydromorphone 0.5–4 mg IV bolus
Followed by an infusion of 0.5–10 mg IV/h titrated to comfort
Benzodiazepines such midazolam may be used for anxiety
Agitated delirium can be managed with neuroleptics such as haloperidol
There is no ceiling to the amount of comfort care medication that can be applied if used with the principles described above REF
Medications that are not primarily prescribed to alleviate pain and suffering should be ceased
Some medications, such as anti-seizure medications should continue, to avoid situations a patient and their family may find distressing.
All invasive lines and tubes should be reviewed and removed if their purpose is not for providing symptom relief and comfort
This includes:
Endotracheal tube or tracheostomy tube
Arterial line
Central line
Vas Cath
EVD
Nasogastric Tube
Indwelling urinary catheter
Common ICU treatments and monitoring should all be reviewed and stopped if their purpose is not for providing symptom relief and comfort
This includes:
Bloods tests including ABGs
CXR
IV antibiotics
IV Maintenance Fluids
Vital sign observations
Vasopressors and inotropes
Oxygen
TEDS and calf compressors
Holistic care of the patient means treating their family
Social Support
Social workers are essential team members in end-of-life care
Families need support with travel, parking, letters of support, finances and many more logistical issues
Communication
> Ensure privacy and continuity of communication.
> Psychological morbidity is reduced when more time is spent with families during conferencing
> Gaining insight on the values of families and their specific needs is essential
Patient / Family Contact
> Families should be allowed to stay with their relatives at during end-of-life care, with breaks to allow for essential nursing care
> Some families will be grateful for even closer contact with their loved one; this may even include having the patient’s partner or children in bed with them
Thoughtful Acts
Families often appreciate special thoughtful acts such as:
> Playing music in the room that the patient likes
> Creating hand prints of their relative before they die
> Cutting some of the patient’s hair for them to have a memory
> Consideration of cultural, spiritual and religious needs is essential at the end of life.
Religious and Cultural Considerations
> Explore what religious or cultural arrangements the patient or their family would want and facilitate
> Recognise that certain cultures will feel differently about death and have specific needs
Awareness
> Other ICU staff and visiting teams should be updated on what’s happening
> Signs on a patient’s room door can help make all staff aware a patients is having end-of-life care
> Signs on door so people know what’s happening
Psychological support
> Should be offered to distressed families
Bereavement support
> Following death this can make a tremendous difference to how relatives cope.
> See more about memory making for relatives here