Dying is a biological process that happens to all living organisms.
During this process all cellular activities and organ functions progressively cease.
The determination of death is an event in that process when it is determined that the process is irreversible.
How this is determined is actually somewhat arbitrary and represents a societal consensus informed by biological understanding.
This is not to dismiss the different cultural and religious perspectives of death which are considered later.
A HISTORY OF DEATH
Death has always had immense cultural, religious and mystical significance to the human race.
From ancient times until the Renaissance there was no understanding of the biology of death.
At a spiritual level, death was when life or the soul departed from the body.

Understanding death at a biological level was only possible after William Harvey
17th century described the circulation of blood and the function of the heart as a pump.
Harvey stated that ‘…the heart is the principle of life…from which heat and life are dispersed to all parts…’.
Under this concept, death was when the heart and circulation stopped.
William Harvey
1578-1657
Pioneering Anatomist and Physiologist
In the 17th Century
Death was when the heart stopped
19th century it was known that during an increase in intracranial pressure respirations suddenly stopped whereas the heart continued to beat for some time.
It was also recognised that the heart could continue to beat if artificial respiration was performed.
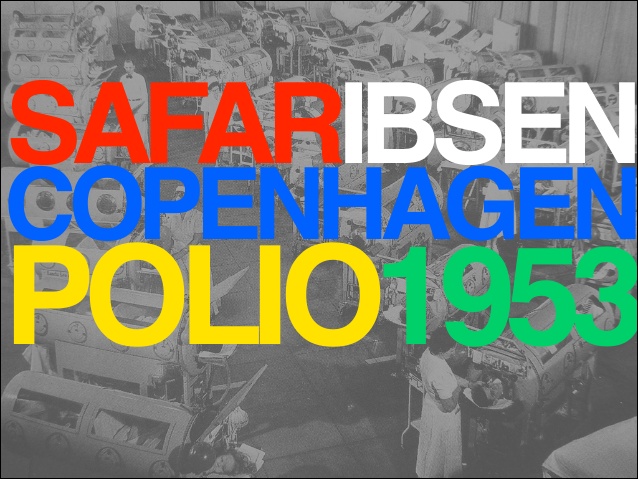
20th Century brought the likes of Peter Safar (arguably the father of modern critical care and ICU) and Bjørn Ibsen who pioneered positive pressure ventilation in ICU during the 1952 Copenhagen polio epidemic.
The success of mechanical ventilation, and the subsequent development of intensive care units (ICUs), rapidly led to positive-pressure ventilation being used in other diseases and conditions, including severe brain injury.
In France in 1959, came the first descriptions of brain death and named it “death of the central nervous system”.
They described this to define criteria for abandoning ongoing intensive therapy.
This artificial construct came about to make physicians comfortable with stopping aggressive therapy
Later in the same year, Mollaret and Goulon in Paris described 23 patients with the same syndrome and called it le coma depassé (literally, beyond coma).
France 1959
The French described brain death
Concept used to stop aggressive therapy
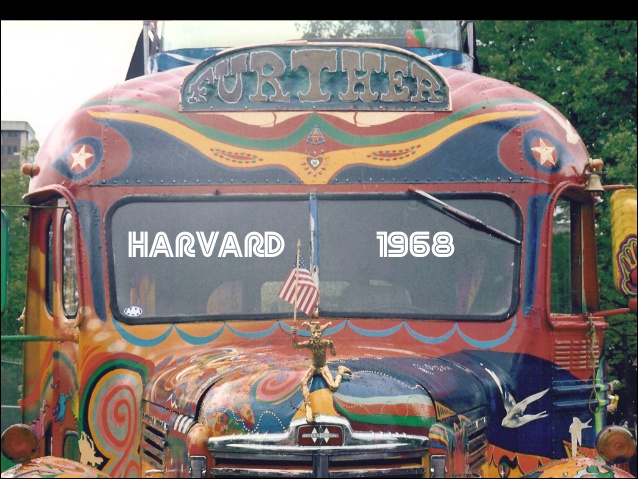
In 1968, an ad hoc committee of Harvard Medical School produced a report on the ‘hopelessly unconscious patient’.
The committee members agreed that mechanical ventilatory support could be withdrawn from patients diagnosed with ‘irreversible coma’ or ‘brain death’ (terms that they used interchangeably) and that, with consent, organs could be removed from such patients for transplantation.
They stressed that their primary concern was to provide an acceptable mechanism to permit withdrawal of mechanical ventilatory support from such patients, and that the sanction this gave to removal of organs for transplantation was secondary.
Lack of precision in the definition of brain death caused considerable confusion in subsequent years.
To deal with this a United States President’s Commission was appointed, which declared in 1981 that individual death depended on either:
- Irreversible cessation of circulatory and respiratory functions or
- Irreversible cessation of all functions of the entire brain
The consequent Uniform Determination of Death Act referred to ‘whole brain death’ as a requirement for the determination of brain death. Subsequently, this declaration has been enacted into law in most states.
The UK in the late 70’s created a statement called Diagnosis of Brain Death outlined a way of diagnosing brain death.
In a move that some find controversial, in 1995 a revised definition changed brain death to brain stem death: irreversible loss of the capacity for consciousness together with the irreversible loss of the capacity to breathe.
This is NOT the definition or nomenclature used in Australia but practically boils down to the same thing.

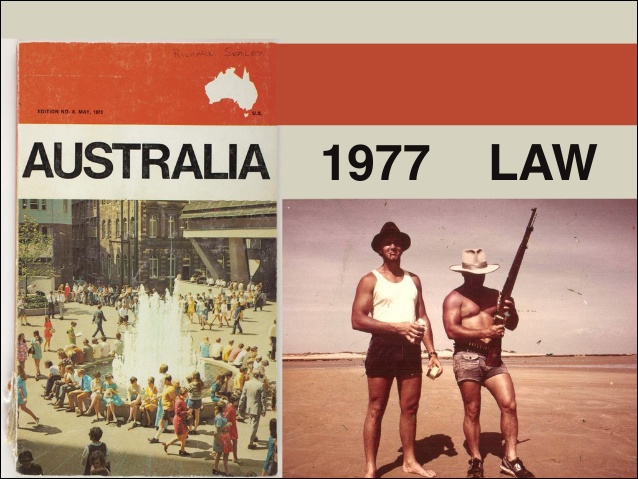
In 1977, the Australian Law Reform Commission addressed the absence of definition of death in Australian law, recommending that a statutory definition of death should be introduced.
They recommended that death be defined as:
- Irreversible cessation of all function of the brain of the person; or
- Irreversible cessation of circulation of blood in the body of the person.
They did not provide detailed criteria, on the grounds that ‘the creation and prescription of techniques of diagnosis should be the responsibility of the medical profession’.
They specified that, although it appeared in the context of transplantation, the definition should have general application.
Current Australian state and territory laws vary, but all are based on the recommendations of the Australian Law Reform Commission.
WHAT FINALLY CAUSES DEATH?
The most common way for death to be certified is when there is irreversible cessation of circulation of blood in the body of a person.
It occurs when the heart stops beating. The person then stops breathing, stops moving and has no pulse.
This is the general public’s most common perception of what death is.
This is the final consequence of all causes of death apart from neurological catastrophes that cause brain death.
In the context of neurological emergencies, if the injury does not cause brain death, a common mechanism for death to occur is neurological impairment affecting respiration and protection of airway reflexes. This may cause hypoxia and subsequently cardiac arrest.
Death may be certified when there is permanent loss of all brain function. This is also called Brain Death.
Overall this is a very rare event – only 2% of hospital deaths REF
It occurs when a neurological catastrophe has occurred, such as TBI, ICH, aSAH, or a severe hypoxic brain injury.
The final consequence causing death in these contexts is that the pressure inside the skull is so high that blood can no longer enter.
This causes ischaemia then death of all brain tissue and irreversible cessation of all functions of the brain, including the brainstem.
The heart may continue to beat and spinal function may persist.
ORGAN DONATION
Organ donation (OD) is when an individual donates one or more if their organs to help someone else in need of that organ.
Live organ donation occurs when someone makes an informed decision to donate a kidney, or more rarely, some of their liver to a suitable recipient. MORE
Organ donation after death can occur if someone wanted to be an organ donor, if they are suitable donor, if there are suitable recipients and if they die in ICU in a controlled manner. All this means OD is rare event, only possible in 2% of hospital deaths REF
If organ donation isn’t possible, tissue donation after death often is.
Discussion with families about organ donation is a routine part of end of life care in ICU. REF
This has changed over the years, and patients who previously would not have been considered for OD now may be.
Essentially, anyone in the Emergency department or ICU for whom there is medical consensus for End-of-Life care should be considered for OD and referred to a donation specialist. REF
This is the safest way to ensure we fulfil the wishes of all patients who would want to be organ donors.
