> Only considered after medical consensus has been reached that active treatment is no longer in the patient’s best interests
> If the patient is deemed medically suitable and there are suitable recipients
> It is expected the patient will die within the required time frame
> Following a Donation Conversation in which a family consent to organ donation
The agonal period is the time from withdrawal of cardiorespiratory support until circulatory arrest
It is limited to approximately 90 minutes in Australia and New Zealand so that if death has not occurred within this time frame the donation process is usually aborted, although other countries accept longer agonal periods (2 hours in Spain, Canada and the Netherlands and 3 hours in the UK).
The functional warm ischaemic time is the time from when the systolic blood pressure falls below 50 mmHg after withdrawal of cardiorespiratory support to cold perfusion and may be a better measure of ischaemic injury REF
Organs have different susceptibility to warm ischaemia with the liver and heart being particularly vulnerable.
A guide to current acceptable ischaemic times in Australia and New Zealand is as follows, although individual donor and recipient factors may influence this on a case-by-case basis.
Australia
Liver, pancreas: <30 minutes from withdrawal of cardiorespiratory support to cold perfusion
Heart: <30 minutes from SBP < 90 mmHg following withdrawal of cardiorespiratory support to cold perfusion
Kidneys: <60 minutes from SBP < 50 mmHg post withdrawal of cardiorespiratory support to cold perfusion
Lungs: <90 minutes from SBP < 50 mmHg post withdrawal of cardiorespiratory support to cold perfusion
New Zealand
Liver: ≤30 minutes from withdrawal of cardiorespiratory support to cold perfusion
Kidneys, Lungs: ≤90 minutes from withdrawal of cardiorespiratory support to death
Predicting the Time Frame of Death
As alluded to earlier, this is difficult
Factors considered when estimating whether they will pass away in this period include:
> Whether they are likely to obstruct their airway (body size, history of OSA, no airway reflexes)
> How well they are breathing – effort and respiratory rate
> How hypoxic they are to start with
> The neurological exam – if they have no cough, no corneal reflexes, no motor response to pain, less likely to survive > 90 minutes REF
How is DCDD actually done?
This is a relatively rare event and requires intensive input from the Donation Specialist staff.
Each institution involved in OD will have a local protocol for how it is done.
This whole process often takes 24 hours
> This includes taking blood samples for serology and tissue typing.
> Other blood tests and imaging may be required to assess donor and organ suitability.
> Liaison with transplant units to determine organs to be retrieved, obtaining of formal consents, arrival of retrieval surgeons and preparation of the operating theatre must all occur before withdrawal of treatment.
> Occasionally the retrieval process can be expedited if the donor is physiologically unstable
It is recommended that a brief meeting of:
Donation staff
Relevant ICU staff
Retrieval team
Operating theatre staff
Occurs prior to cardiorespiratory support being withdrawn.
This meeting should cover the specifics of the situation, so that all personnel are aware of the plan and their individual responsibilities and are prepared for them.
The time and place of withdrawal of cardiorespiratory support is negotiated by the intensivist and donation staff with the donor family, the retrieval surgeons, the operating theatre and ICU staff.
Withdrawal of cardiorespiratory support may occur in three different locations.
In the ICU
> This provides the maximum opportunity for family members to be with the patient, including at the time of death
> The patient is not moved to the operating theatre until immediately after death
> If death does not occur within the predetermined time frame in which organ donation is feasible, unnecessary patient movement is avoided
> However, if death does occur within such a time frame, rapid transfer of the deceased patient to the operating theatre is required
> In some instances, the additional warm ischaemic time may make some organs (e.g. the liver) unsuitable for transplantation
In an appropriate room near the operating theatre
> Involves moving the living patient but enables similar family access to the patient at the time of withdrawal of cardiorespiratory support as would occur in the ICU
> Reduces the time between death and organ removal
> Still requires rapid transfer of the deceased patient to the operating theatre if death occurs within the predetermined time frame
> Requires transfer back to the ICU if this does not occur
In the operating theatre
> Requires moving the living patient and may limit family access at the time of death
> Requires the return of the patient to the ICU should death not occur in the predetermined time frame
Essentially they are not involved until the patient is certified dead and the ICU staff and family leave
It’s recommended that ICU staff should not witness the post-mortem process of organ removal
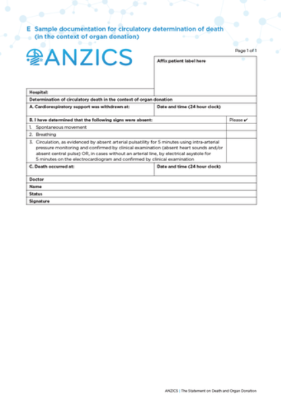
> Arterial line monitoring is the recommended method to determine the loss of pulsatile arterial blood pressure in the context of donation.
> Absent pulse on the arterial line for 5 minutes is observed and then confirmed by clinical examination (absent heart sounds and/or absent central pulse).
> Reliance on an isoelectric ECG may unnecessarily prolong the observation period so the ECG should not be monitored if an arterial line is present.
7% of patient have ECG activity for greater than 30 minutes post cessation of a pulsatile arterial blood pressure
> When the use of an arterial line is unacceptable to the patient or family or is not technically possible, electrical asystole must be observed for 5 minutes on the ECG. Absent circulation is then confirmed by clinical examination (absent heart sounds and/or absent central pulse).
The family must be informed; they are often with their relative after withdrawal of life support so will know as it happens.
The patient then continues end-of-life care in ICU as they would do otherwise.