Spinal Cord Injury (SCI) specifically refers to damage to the cord, as opposed to bony or ligamentous spinal injuries.
It may be traumatic or non-traumatic.
Global incidence: 13/100,000. This is about 30 times less common than TBI.
Global prevalence: 368/100,000. Only half that of TBI

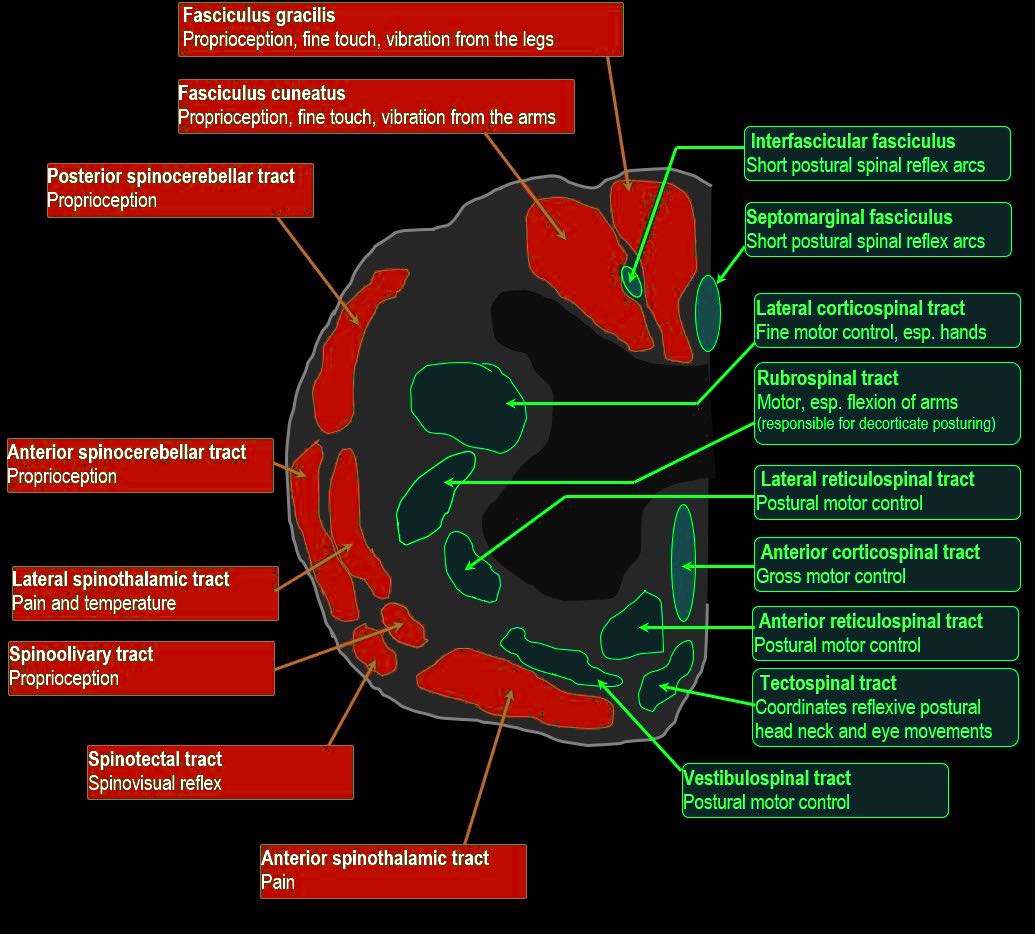
CLINICALLY RELEVANT ANATOMY
With permission from Andy Neill
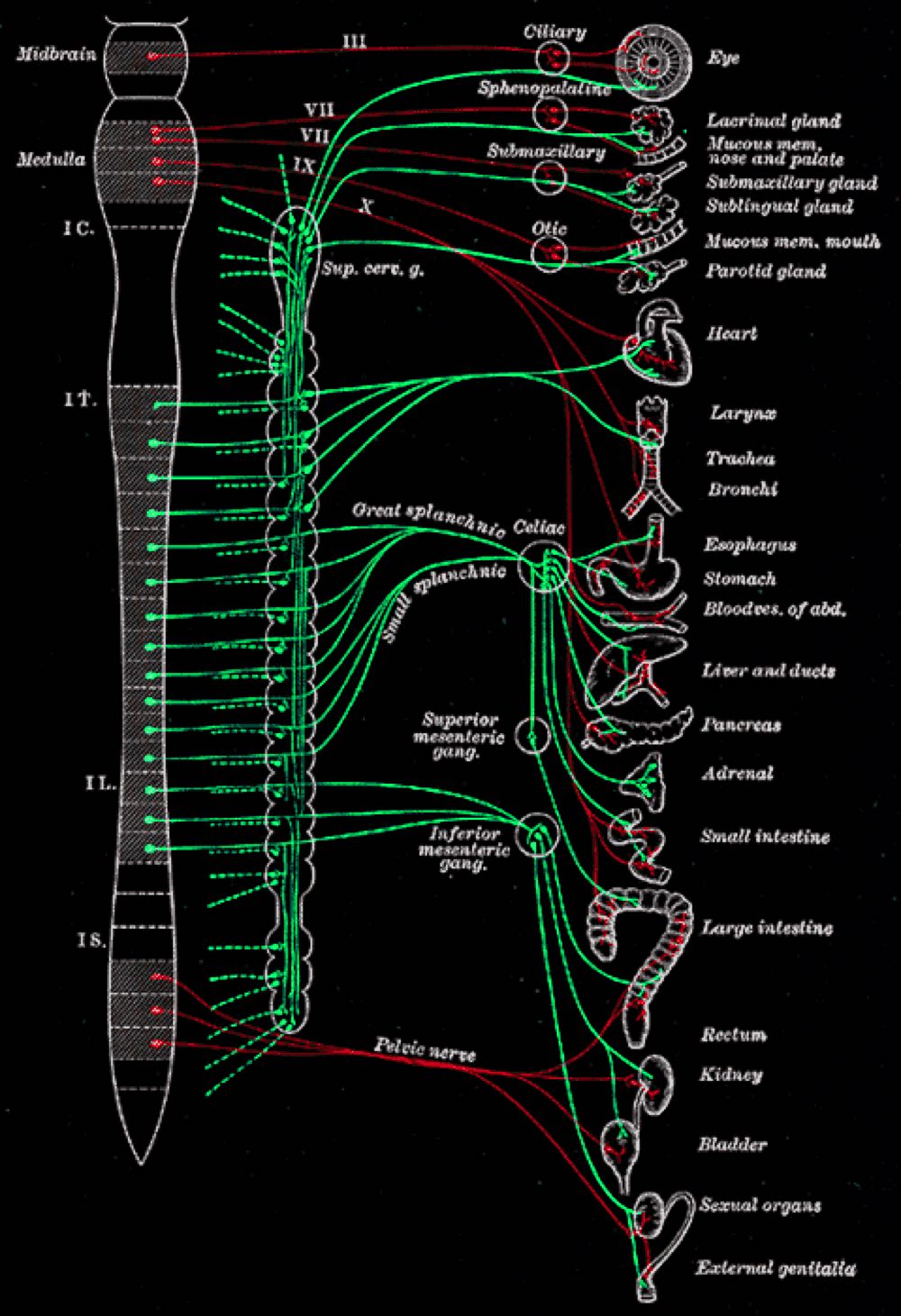
CC CREDIThttps://en.wikipedia.org/wiki/Autonomic_nervous_system#:~:text=The%20autonomic%20nervous%20system%20is,%2C%20urination%2C%20and%20sexual%20arousal.
CLINICAL RELEVANCE?
Cervical SCI is below where visceral parasympathetic innervation comes out via the vagus, but above the thoracic sympathetic outflow.
Therefore after cervical SCI there is unopposed parasympathetic innervation to most organs, i.e. the opposite of the flight /fight response.
This leads to:
> Hypotension (loss of vasomotor tone and less endogenous catecholamine production)
> Bradycardia (loss of cardiac sympathetic innervation T1-4)
> Bronchospasm (unopposed parasympathetic innervation of lungs causes bronchoconstriction)
> Thick secretions (unopposed parasympathetic innervation of lungs causes thick, tenacious sputum)
> Urinary retention (paralysis of detrusor muscle, loss of bladder stretch sensation)
> Gastroparesis (unopposed parasympathetic innervation of bowel)
> Increased gastric acid production (unopposed parasympathetic innervation of bowel)
> Priapism (unopposed parasympathetic innervation of genitals)

The primary muscle of inspiration is the diaphragm, innervated by C3,4 and 5 via the phrenic nerve. Contraction of the diaphragm pushes the abdominal contents down, thus expanding the superior/inferior dimension of the thorax. The compressed abdominal contents are also pushed anteriorly, dragging the ribs with it and thus expanding the anterior/posterior thoracic dimension.
The next most important muscles of inspiration are the upper and more lateral external intercostals, and the parasternal portion of the internal intercostal muscles. Both the external intercostal muscles and the parasternal portion of the internal intercostal muscles elevate the ribs.
The sternocleidomastoid, the scalenes (anterior, middle, and posterior) and pec. major are “accessory muscles of respiration”; they assist in elevating the rib cage and play a more important role in high SCI when other muscles of respiration are paralysed, and the medial part of pectoralis major becomes important for expiration.
In expiration the most important muscles are those of the abdominal wall (including the rectus abdominus, internal and external obliques, and transversus abdominus), which drive intra-abdominal pressure up when they contract, and thus push up the diaphragm, raising pleural pressure, which raises alveolar pressure, which in turn drives air out. This is most important as part of the cough reflex, necessary to clear secretions. The internal intercostals also assist with active expiration by pulling the ribs down and in, thus decreasing thoracic volume.
Note: the intercostal and abdominal musculature are innervated by motor fibres that come from the spinal cord lower down, at their spinal level. So a SCI at C7 will leave the diaphragm intact but the intercostal and abdominal muscles paralysed. At C4, there may be some diaphragmatic movement but full power is unlikely. At C2 there is no diaphragmatic movement.
More on the anatomy and physiology of breathing
REMEMBER
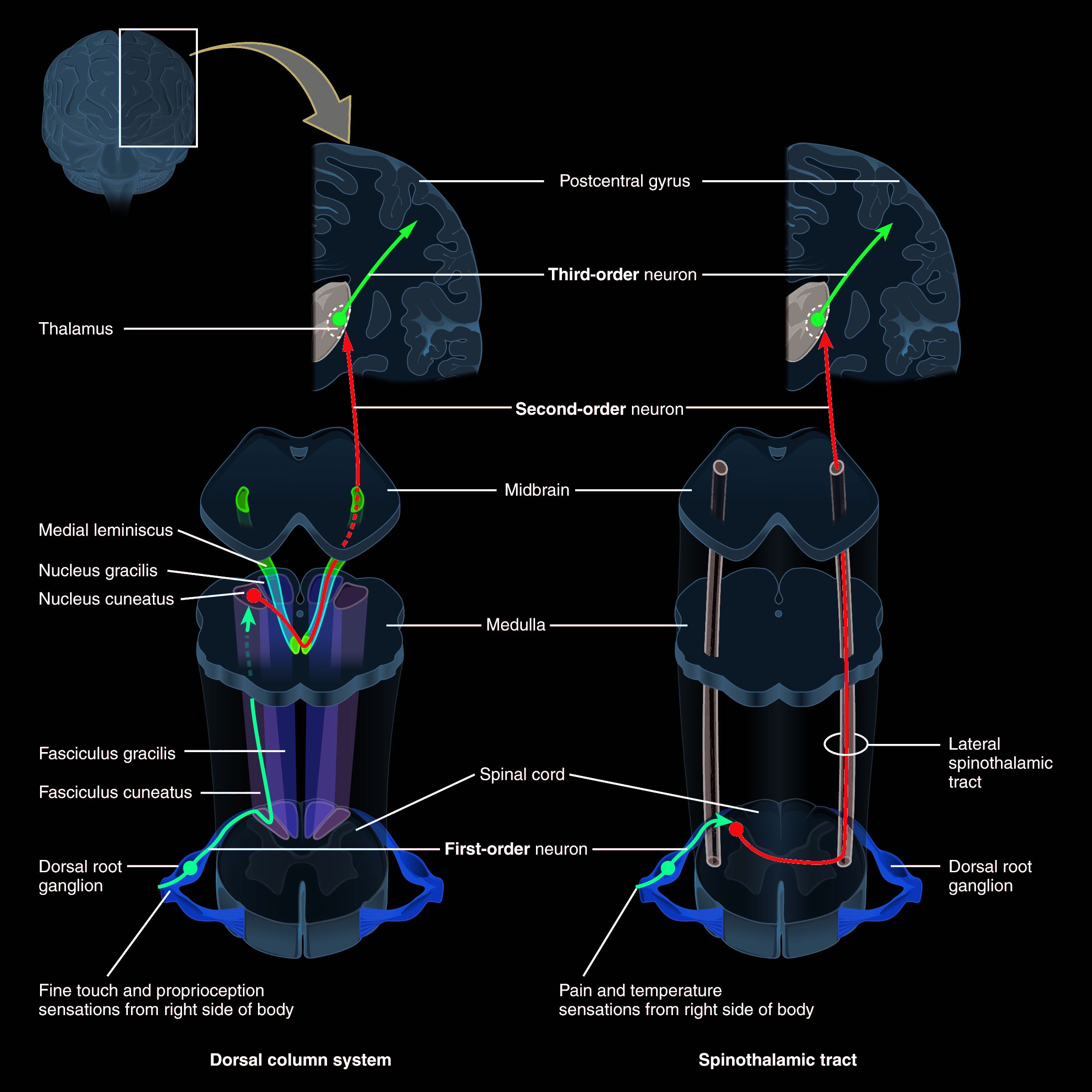
The ascending pathways carrying fine touch, vibration and proprioception only cross over up in the medulla.
The ascending pathways for crude touch and pressure and pain and temperature cross after 1-2 vertebral levels.
The descending motor pathways cross high, in the medulla.
This matters when there is damage to one half of the spinal cord (Brown-Sequard syndrome)
CLINICALLY RELEVANT PATHOPHYSIOLOGY
In TSCI, direct mechanical injury may produce focal compression, laceration or traction injury to the cord.
Actual transection is unusual.
Ischaemic injury may result from interference to the segmental spinal arterial supply.
Initial pathological changes include the traumatic severing of axons, blood vessels and cell membranes
In NTSCI, the commonest mechanisms of primary injury are:
> Compression/contusion – e.g. disc prolapse, tumour, extradural abscess
> Inflammation – e.g. infection, transverse myelitis, MS, radiation
> Ischaemia – e.g. aortic dissection, thromboembolic events
> Intracellular defects – e.g. metabolic defects, genetic disorders, congenital disorders
More NTSCI aetiology classification here
Local ischaemia begins at the site of injury, extending progressively over hours from the site of injury in both directions.
There is loss of autoregulation of blood flow to the spinal cord, often complicated by arterial hypotension in high SCI.
Apart from ischaemia, other mechanisms may contribute to the secondary injury, including release of free radicals, reactive oxygen species, eicosanoids, calcium, proteases, phospholipases and excitotoxic neurotransmitters (e.g. glutamate)
Petechial haemorrhages begin in the grey matter, progress over hours and may result in significant haemorrhage into the cord.
There is oedema, cellular chromatolysis and vacuolation, and ultimately neuronal necrosis.
Apoptosis, especially of oligodendrocytes, also occurs.
In the white matter vasogenic oedema, axonal degeneration and demyelination follow.
Polymorphs infiltrate the haemorrhagic areas.
Late coagulative necrosis and cavitation subsequently take place.
The resulting time course is:
- Hours – days: inflammation, oedema, increased BBB permeability, haemmorhage, demyelination and cell death
- Days – weeks: resolution and initial repair
- Months – years: gliosis, further demyelination and syrinx formation in up to 30%, but also adaptive functional plasticity through preserved axons
CLINICAL RELEVANCE
> Avoiding hypotension and hypoxia is essential to prevent unnecessary ischaemia and further neuronal death
> Hypertensive therapy aiming for MAP >85 for 5-7 days may improve perfusion of threatened neurons, see management section