WHY BOTHER WITH ISNCSCI?
Whilst a standard neuro exam should help diagnosis of SCI, using the standardised ISNCSCI classification has additional advantages:
> Most validated instrument for diagnosing and classifying SCI
> Only exam that allows prognostication which patients and families often ask about
> Sufficient inter-rater reliability for local and international data collection / comparison
In brief, it gives a neurological level of injury which dictates much about expected function, and a grade, which implies completeness, severity and probability of improvement.
HOW TO DO THE ISNCSCI
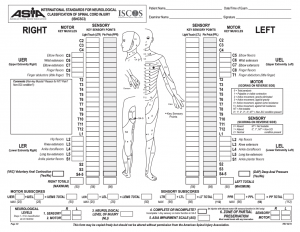
Determine sensory levels for right and left sides.
The sensory level is the most caudal (lowest), intact dermatome for BOTH pin prick AND light touch sensation
WATCH OUT!
The “Cervical Cape” is not fixed, meaning the C4 dermatome can scoop down, often to the level of the nipples
Test T2/3/4 laterally to avoid being tricked
It’s common to see sensory level documented as T4 and motor C5, when reality is both are C5

Determine motor levels for right and left sides.
Defined by the lowest key muscle function that has a grade of at least 3 (on supine testing), providing the key muscle functions represented by segments above that level are judged to be intact (graded as a 5).
Note: in regions where there is no myotome to test, the motor level is presumed to be the same as the sensory level, if testable motor function above that level is also normal.

Determine the neurological level of injury (NLOI).
This refers to the most caudal (lowest) segment of the cord with intact sensation and antigravity (3 or more) muscle function strength, provided that there is normal (intact) sensory and motor function rostrally respectively.
The NLI is the most cephalad (highest) of the sensory and motor levels determined in steps 1 and 2.
Determine whether the injury is Complete or Incomplete.
i.e. absence or presence of sacral sparing
If NO voluntary anal contraction AND all NO S4-5 sensation then injury is Complete
Otherwise, injury is Incomplete.
Determine ASIA Impairment Scale (AIS) Grade.
Is injury Complete? If YES, AIS=A
If NO – Is injury Motor Complete? If YES, AIS=B
If not motor complete, are half or more of the key muscles below the neurological level of injury graded 3 or better?
No: AIS=C (i.e. most myotomes <3/5)
Yes: AIS=D (i.e. most myotomes >/= 3/5)
If sensation and motor function is normal in all segments, AIS=E
Note: AIS E is used in follow-up testing when an individual with a documented SCI has recovered normal function.
If at initial testing no deficits are found, the individual is neurologically intact and the ASIA Impairment Scale does not apply
The ZPP is used only in complete SCI (ASIA A)
It refers to those dermatomes and myotomes caudal (lower) to the sensory and motor levels that remain partially innervated.
With sacral sparing of sensory function, the sensory ZPP is not applicable and therefore “NA” is recorded in the block of the worksheet.
Accordingly, if VAC is present, the motor ZPP is not applicable and is noted as “NA”
SCI SYNDROMES
Weakness and sensory loss, greater in the arms than the legs.
Typically follows a hyperextension injury with pre-existing canal stenosis, such as an elderly man falling onto his chin.
Ischaemia or haematoma in the centre of the cord affect the cervical segments more due to the pattern of lamination of the corticospinal and spinothalamic tracts.
Loss of motor function and pain and temperature sensation below the NLOI, with preservation of fine touch and proprioception.
Less common, typically following interruption of the blood supply to the anterior spinal cord.

Ipsilateral loss of motor, proprioception and fine touch, with contralateral loss of pain and temperature sensation below the NLOI.
Usually follows a penetrating SCI damaging only one half of the spinal cord.
Sudden onset, symmetrical paraplegia with mixed upper and lower motor neuron findings, caused by injury at T12/L1.
Often asymmetrical, lower motor neuron lower limb weakness with saddle area hypoaesthesia or paraesthesia, with bladder and bowel areflexia.
Caused by injuries below L1 damaging the lumbosacral nerve roots.