
OUR CASE
Michael
If initial SBP 150-220 mmHg, target NI SBP 130-150 mmHg
If initial SBP > 220 mmHg, target NI SBP 140-180 mmHg
Ensure coagulation normalised
Manage EICP
Have low threshold to re-image
Surgery if indicated, particularly for HCP or posterior fossa ICH
Look for and treat underlying cause
Look for and treat seizures
Avoid hyperthermia
Euglycaemia
Start chemical VTE prophylaxis day 1-4 when haematoma has stopped expanding
Monitor for swallowing dysfunction
A BIT MORE DETAIL…
Neurological observations include:
- GCS assessment and motor strength.
- NIHSS every 4 hours
Changes in neurological observations must be escalated promptly as it may represent a time-dependent emergency e.g.
Haematoma expansion
Now Intraventricular hameorrhage
Hydrocephalus
New clot formation and vessel occlusion
Worsening cerebral oedema with mass effect
- Reduced level of consciousness, fluctuations or a change in Glasgow Coma Score
- Pupillary changes – unequal, dilated, pinpoint or non-reactive to light
- New onset or worsening of a neurological deficit such as weakness in the face, arm or leg down one side of the body, as well as problems with swallow, speech, sensation or vision.
- A change in the NIHSS score
- Severe headache
- Nausea and vomiting
- Blood pressure out of target range
Continuous pulse oximetry to ensure hypoxia is prevented
Cardiac telemetry, at risk of dysrhythmia
Invasive and non-invasive blood pressure monitoring
If EVD in situ for HCP or EICP:
ICP
Amount of fluid drained per hour and 24hs
CSF analysis twice weekly
If presenting SBP 150-220 mmHg, aim Non-Invasive SBP 130-150 mmHg
Try to lower BP smoothly
Start treatment within 2 hours
Achieve target within 1 hour of starting
Avoid variability
> Arterial line usually essential
> Central line often required
If initial SBP > 220 mmHg, aim SBP 140-180 mmHg
– Some evidence of increased harm in rapid reduction of BP in this group
How to achieve this?
Treat pain first (especially in intubated patients, elevates BP)
Use titratable IV agents as per your local institutional guideline
> Remember SMOOTH, MINIMAL VARIABILITY
Bolus doses e.g.
- IV hydralazine 10 mg q15 min
- IV labetalol 20 mg over 2 minutes
- IV metoprolol 5 mg over 5 minutes
Infusions e.g.
> Clevidipine a newer dihydropyridine calcium-channel blocker that has a short half life may be given via continuous infusion and is easily titratable
> Avoid GTN, ideally avoid sodium nitroprusside too; these are venodilators and can potentially increase ICP and potentially haematoma growth.
Repeat coagulation profile
Treat thrombocytopenia, aim Plt > 100K if possible
ASPIRIN or CLOPIDOGREL
Don’t give platelets UNLESS neurosurgery happening
No evidence for desmopressin (DDAVP)
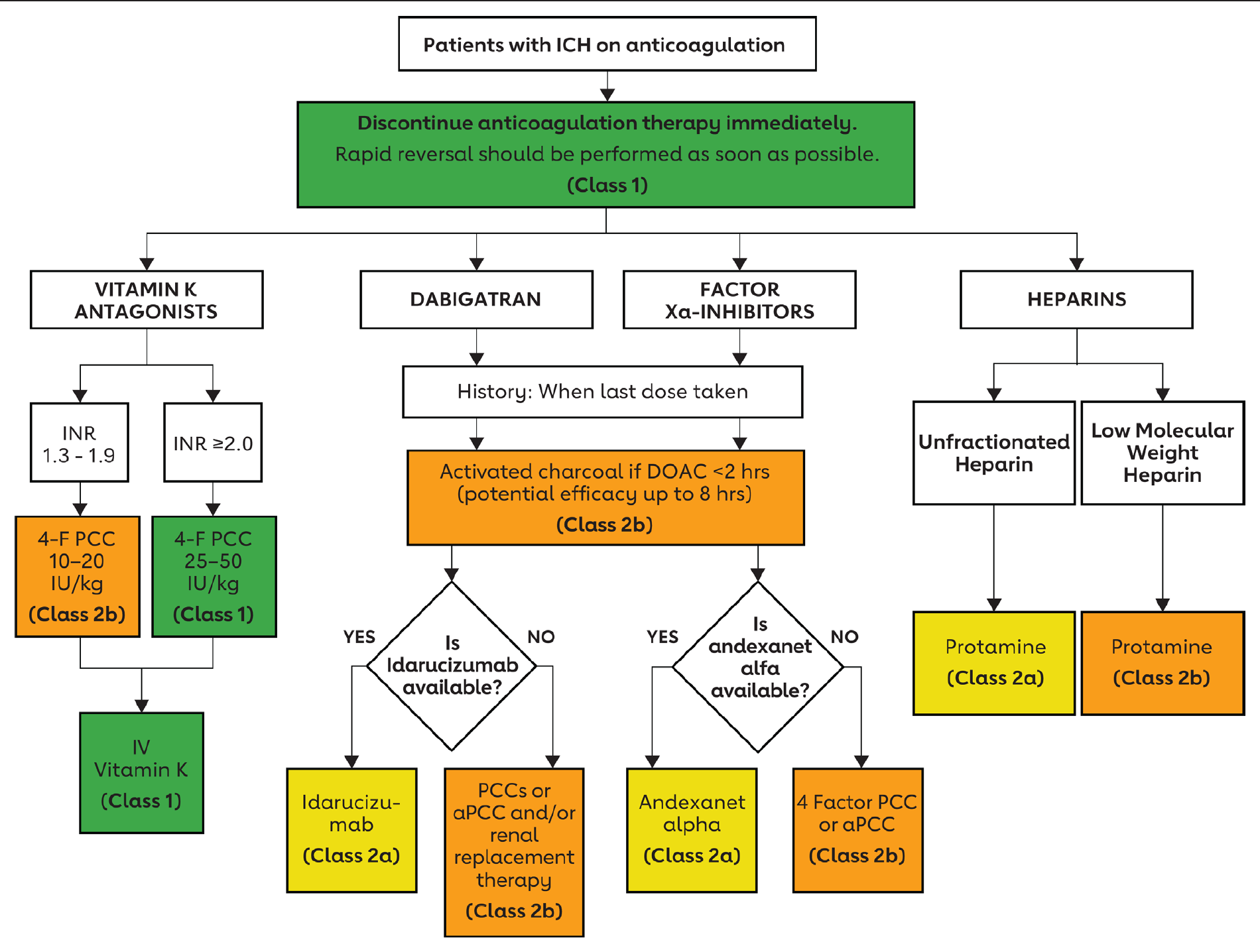
Warfarin
4 Factor PCC better than FFP
Also give 10 mg Vit K
Dabigatran
Consider idarucizumab 5 g, provided as two separate vials each containing 2.5 g/50 mL idarucizumab
Activated charcoal (50 gm) should also be given if ICH occurs within 2 hours of most recent dabigatran dose.
If idarucizumab is not available, consider activated PCC
These approaches do not fully reverse dabigatran
Direct Xa inhibitors
(Rivaroxaban, apixaban, edoxaban, betrixaban)
Andexanet alpha
Dosing depends on which agent
Activated PCC
Heparins (unfractionated or LMWH)
Protamine
PROTHROMBOTICS
No current evidence or recommendation for Recombinant Factor VIIa or TXA
Occur in up to 8-20% most in 1st 24 h
Lobar ICH a risk factor
Non-convulsive seizures more common than convulsive
These may be associated with expanding haematoma
Have low threshold to obtain EEG
Consider continuous EEG in unconscious patients if available
If seizure (clinical or electroencephalographic) seen, treat.
Levetiracetam 1st agent of choice
Prophylactic ASMs not recommended but that was based on when phenytoiun was ASM usually used
Risk / benefit of prophylactic levetiracetam unknown.
BLOOD GLUCOSE MONITORING & CONTROL
- BGL should checked on admission to ICU and every 6 hours thereafter
- BGL should be maintained 6-10 mmol/L
Fever is common after ICH and is associated with poorer outcomes.
It occurs in 1/3 of patients.
Of these, 2/3 have do not have an infective source found REF
Cultures should be taken, including from CSF.
Antibiotics are usually not given unless there is a clear source or other signs of sepsis
Antipyretic therapy, comprising regular paracetamol or physical cooling measures should be used routinely where fever i.e. temperature> 37.5 degrees occurs
There is no evidence for routine hypothermia for ICH
All patients receive intermittent pneumatic compression stockings
Elastic compression stockings are not used
In non-ambulatory patients, low-dose UFH or LMWH prophylaxis at 24 to 48 hours from ICH onset is reasonable
It may be reasonable to first document haemorrhage stability on CT if LMWH prophylaxis is started in the 24- to 48-hour window after ICH onset.
One approach from a Finnish group:
SMASH-U
Further Investigations
CTA +/- Venogram:
- To exclude underlying vascular malformation, aneurysm (rare cause of ICH), tumor (which is usually better diagnosed on contrast MRI), Moya Moya, vasculitis or cerebral sinus thrombosis.
- Perform for
- Lobar spontaneous ICH if age < 70
- Deep/ post fossa ICH and age < 45
- Deep/ post fossa ICH, age 45-70 and no history of hypertension
- In these patients, if CTA/CTV negative, then do a MRI/MRA
- If MRI/MRA negative, then consider DSA
MRI / MRA
- To investigate for underlying vascular malformations / tumour
- Reveals cerebral amyloid angiopathy better than CT
- In patients with spontaneous ICH and a CTA or magnetic resonance angiography (MRA) suggestive of a macrovascular cause, catheter intra-arterial DSA should be performed as soon as possible to confirm and manage underlying intracranial vascular malformations.
DSA
- See above
- If intra-ventricular haemorrhage (IVH) and no detectable parenchymal haemorrhage
- If all investigations negative including DSA, consider repeating DSA in 3-6 months
DYSPHAGIA & NUTRITION ASSESSMENT
All stroke patients are to be kept ‘Nil By Mouth’ (NBM) until swallow assessment performed (e.g. ASSIST Screen)
If patient fails the assessment, they should be kept NBM until Speech Pathology review.
An NGT may be inserted 8 hours following administration of rt-PA, although it may be more appropriate to wait until 24 hours in the absence of significant underlying nutritional risk or essential oral medications (e.g. Parkinson’s disease medications), particularly where NGT insertion is anticipated to be difficult.
A specific situation, often highly charged
Patients who show evidence of haemorrhage following rtPA warrant consideration of rtPA reversal in select cases.
Thrombolysis is not easily reversed but guidelines suggest:
Cryoprecipitate as soon as possible after detection of sICH with empirically transfusing with 10 U cryoprecipitate and anticipate giving more cryoprecipitate as needed to achieve a fibrinogen level of ≥150 mg/dL.
Platelet transfusion is not routinely recommended except in those with thrombocytopenia (platelet count <100 000/μL).
Use of 4-factor PCC/ prothrombin complex concentrate is recommended in patients on warfarin treatment before getting tPA (those with a sub therapeutic INR who qualified for IV thrombolysis). PCC is the preferred modality, but if unavailable, fresh frozen plasma may be used. Adjunctive therapy with vitamin K should also only be reserved for this subgroup that was on warfarin before receiving alteplase.
Antifibrinolytics have limited data but should be considered in patients with sICH, particularly in patients who decline blood products.
Given lack of safety data, use of activated factor VIIa is not recommended.
Patients should have BP parameters reviewed and managed like other ICH patients.
Clear Neurosurgery Indications
Posterior Fossa (cerebellar) haemorrhage
If:
- GCS </= 13
- Haematoma > 4 cm
- Hydrocephalus
- Brain stem compression
Hydrocephalus
Often due to extension of ICH to IVH
> Indication for an External Ventricular Drain (EVD)
Poor prognostic sign if this is required
> Avoid an EVD for HCP from cerebellar ICH – this may cause upward herniation. Evacuate clot instead, +/- EVD.
Less Clear Indications
Evidence is lacking to support surgery for supratentorial ICH.
The STICH Trial was an RCT comparing medical management with early haematoma evacuation. It showed no benefit from surgery.
The STICH-II Trial looked specifically at superficial lobar ICH. Again there was no benefit from surgery.
There has been much debate about what these studies mean and many neurosurgical centres continue to perform surgery for supratentorial ICH
The reason that these studies showed no benefit may be because some patients benefited and some were harmed.
A recent meta-analysis of all the data suggested surgery was harmful for small lesions with increasing benefit for larger volumes (up to a point) and was beneficial for patients with a GCS 10-13 but not for more or less conscious patients.
A modern neurosurgical textbook suggests consider evacuation if:
- Superficial lobar ICH (not basal ganglia / thalamus ICH)
- There’s marked mass effect (with oedema and midline shift)
- Symptoms are due to mass effect rather than brain injury from the ICH
- Volume 10-30 ml
- Refractory EICP
- Rapid deterioration
- <50 years old
- < 24 hours from onset
Minimally Invasive Surgery
Emerging evidence suggests that minimally invasive surgery could be more promising (with several ongoing trials)
Listen to this talk on the EVACUATE trial, a randomized controlled trial of ultra-early, minimally invasive, haematoma evacuation versus standard care within 8 hours of intracerebral hemorrhage.

Scenario test question

 REF
REF