The clinical features of EICP include:
WHAT CAUSES UNCONSCIOUSNESS?
Overview here
e.g.
The definitive causes of altered consciousness are not known. Loss of consciousness requires either loss of the function of both cerebral hemispheres or of the reticular activating system. Several plausible hypothetical mechanisms have been proposed for the alteration of consciousness that occurs with mTBI. These include the reticular, pontine-cholinergic system, centripetal, and convulsive hypotheses. The reticular activating system (RAS) resides in the brainstem reticular formation which extends from the top of the spinal column to the rostral midbrain with extensions into the thalamus and hypothalamus. The RAS is excited by input from surrounding sensory tracts and transmits this excitation to the cortex to induce generalized cortical and behavioral arousal. In the absence of input from the RAS, consciousness is impaired.
Under the reticular hypothesis of concussion, loss of consciousness after brain trauma results from a disturbance or depression of the activity of polysynaptic pathways within the RAS 25. It is not completely understood how a traumatic dysfunction of the RAS occurs however it is believed to result from shearing or tensile strains on RAS pathways at the cranio-cervical junction. Neuropathological evidence for this is limited.
Potential manifestations of an occulomotor nerve (CN III) palsy include:
- Pupillary dilation
- ‘Down and out’ gaze
- Ptosis
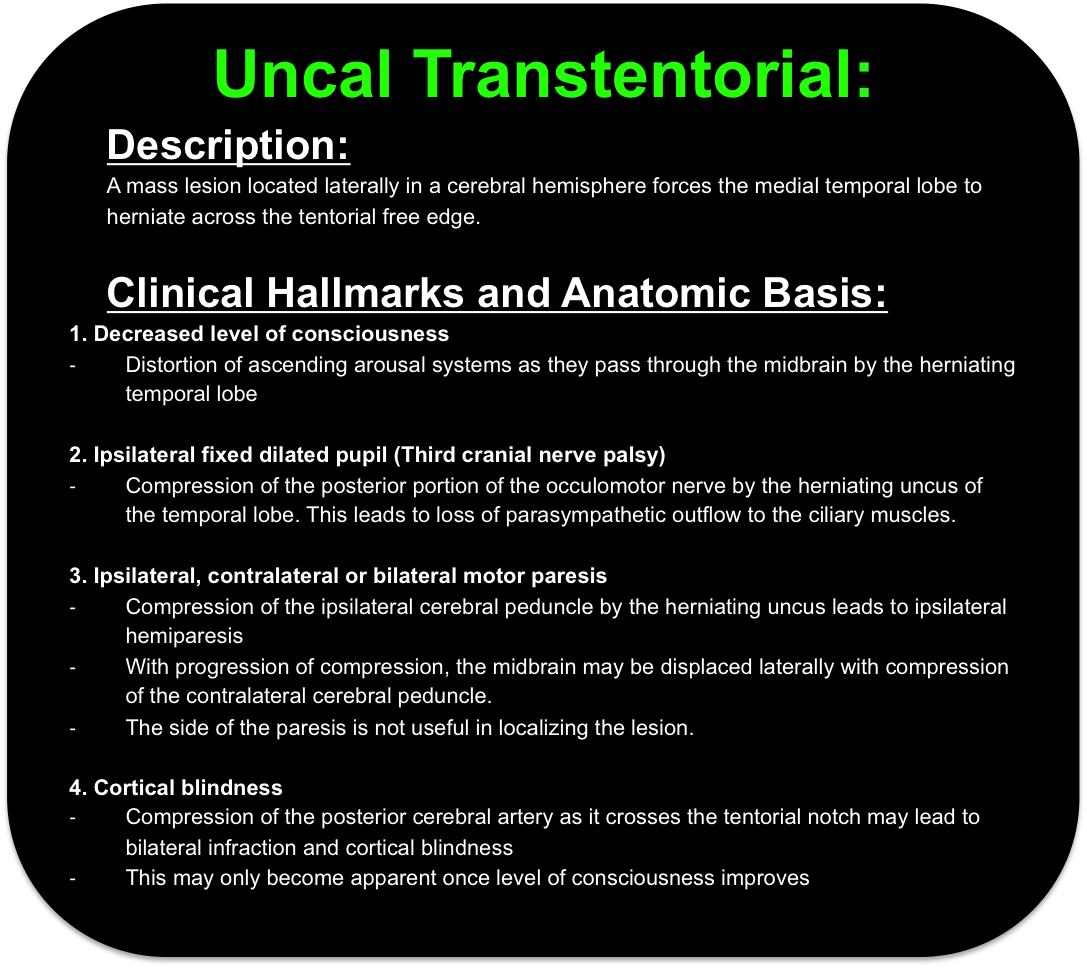
The pupillary sphincter and ciliary muscles are controlled by parasympathetic fibres travelling on the superficial surface of the CN III from the Edinger-Westphal nucleus. Pupillary dilation (unilateral or bilateral) occurs when the CN III’s superficial parasympathetic fibers supplying the ciliary muscles are compressed against the petroclinoid ligament or by uncal herniation.
The ‘down and out’ gaze occurs as a result of impairment of the deep motor fibres of the CN III. This may represent chronic microvascular injury of the small penetrating vessels to the deep motor fibers by diseases such as diabetes, hypertension and atherosclerosis. These pathologies are generally ‘pupil sparing’.
The levator palpebrae superioris is supplied by the superior division of the third cranial nerve. Specifically, superior divisional CN III palsy has been described in association with craniotomy, basilar apex, superior cerebellar, and posterior cerebral artery aneurysms, meningitis, diabetes mellitus, sphenoid sinusitis, ophthalmoplegic migraine, and a postviral illness.
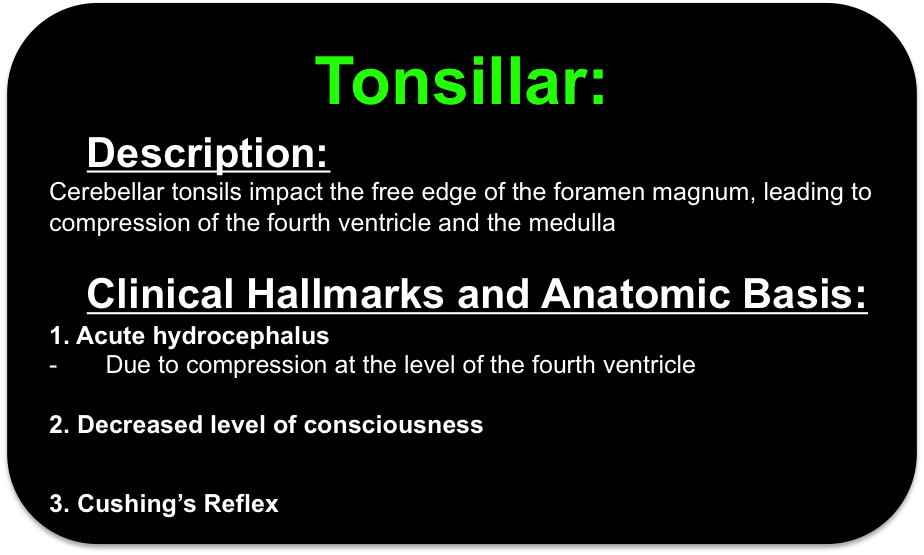
The triad consists of hypertension, bradycardia and an abnormal breathing pattern. The reflex represents central chemoreceptors responding to poor cerebral perfusion with hypertension, which consequently leads to reflex bradycardia. This is considered a late sign
The normal direction of axoplasmic and retinal venous flow in the optic nerve is from the retina towards the cavernous sinus. Engorgement leads to blurring of the margins of the optic disc on fundoscopy and the development of a scotoma.
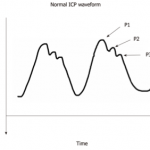
An exaggerated P2 greater than P1 may indicate poor intracranial compliance
- Widespread giant inverted T waves
- QTc prolongation
- ST segment elevation or depression
- Rhythm disturbances
Top clinical signs of EICP
- Pupillary dilatation (unilateral or bilateral)
- Asymmetric pupillary reaction to light
- Decerebrate or decorticate posturing (usually contralateral to blown pupil)
- Progressive deterioration of the neurologic exam not attributable to extracranial factors
The potential radiological features of raised ICP on non-contrast CT brain include:
- Effacement of the ventricles, basal cisterns and other CSF containing spaces
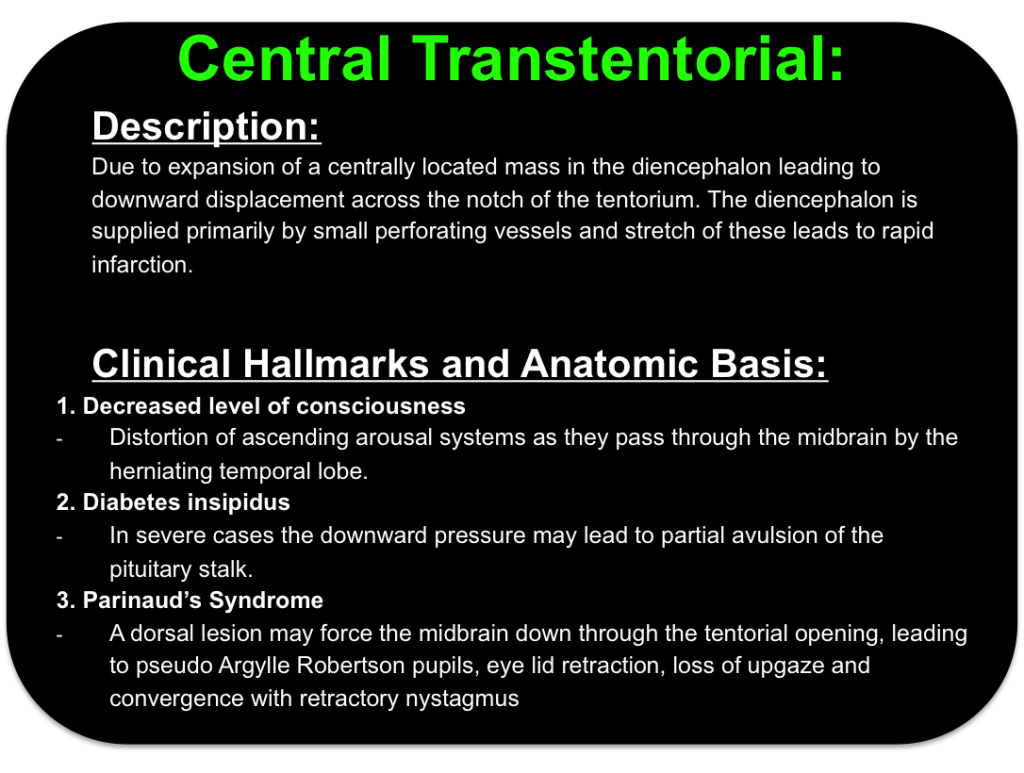
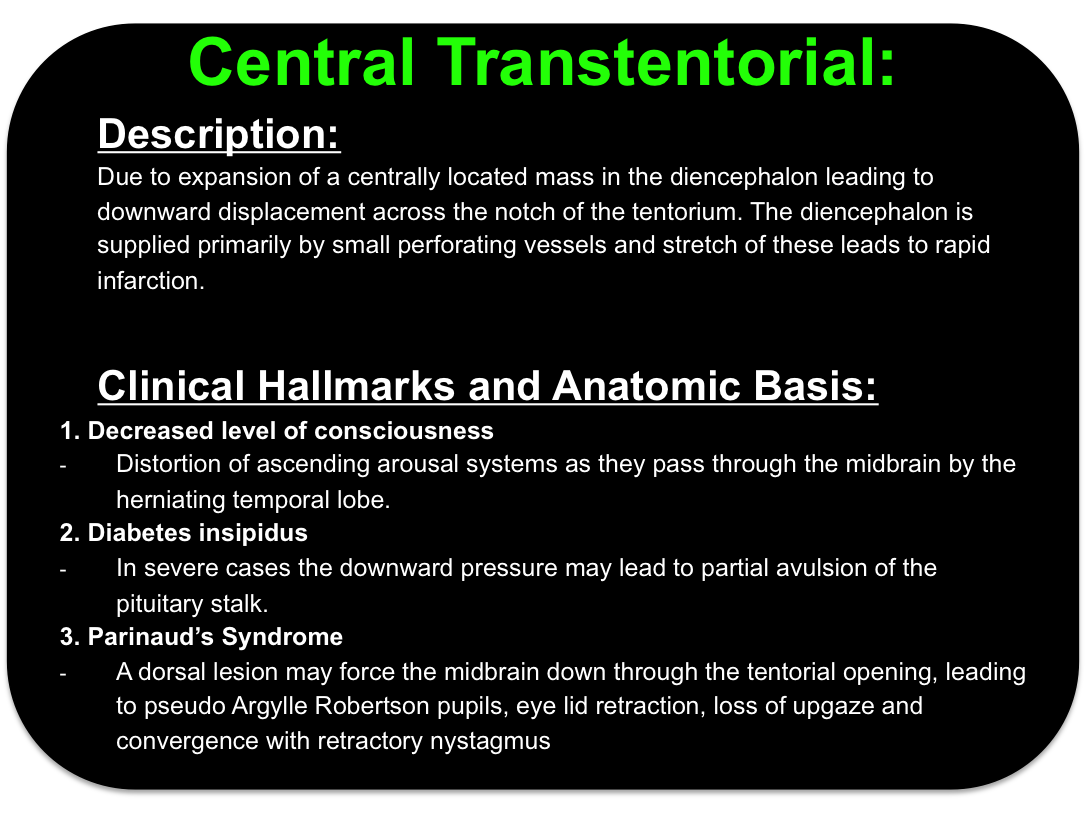
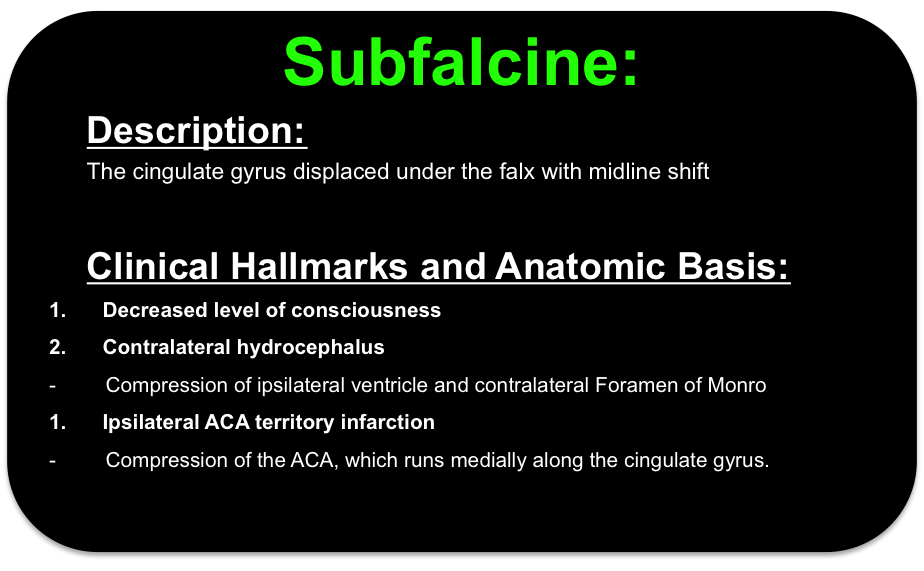
- Brain herniation
- Loss of grey-white matter differentiation