OUR CASE
Katherine was resuscitated in the emergency department and then taken to theatre to have an EVD inserted to manage her hydrocephalus.
A digital subtraction angiogram showed an anterior communicating artery aneurysm amenable to coiling and this was performed with a good result.
When to secure an aneurysm?
As soon as possible, ideally within 24 hours, for the following reasons:
- Coiling/clipping significantly reduces risk of early rebleed (15% within 24 hours for unsecured ruptured aneurysms)
- 1/3 of rebleeds occur within 3 hours
- 1/2 of rebleeds occur within 6 hours
- After the first day, the subsequent risk is 1.5% daily for 13 days
- Facilitates treatment of any future vasospasm by allowing higher arterial blood pressure and volume expansion without danger of aneurysm rupture
- Reduction in overall patient mortality and reduced likelyhood of severe neurological deficit with early intervention (see here)
Endovascular vs surgical management
Therapeutic options include:
1. Endovascular management by interventional neuroradiology
-
- Thrombosis of the aneurysm via coiling is most commonly used.
- Thrombosis by flow diversion, trapping and proximal ligation are other endovascular strategies for securing aneuryms (though less commonly used)
2. Microvascular neurosurgical intervention
-
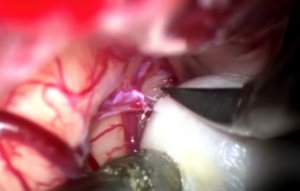
- “Clipping” is the surgical gold standard and by far the most common strategy to secure and aneurysm surgically
- Other methods including wrapping or coating the aneurysm (not preferred and less common)
Clipping vs coiling


Clipping vs coiling
- Treatment choice will depend on aneurysm and patient characteristics
- Multi-disciplinary decision ideally made at centre where both options feasible within 24 hours of ictus
- There have been four major trials conducted comparing the two methods. The largest of these (ISAT 2002) suggested coiling is preferable (if feasible) due a reduced risk of poor outcome (MRS >2; ARR 7%)
- Other factors to consider include
- Technical complications: higher in clipping (19% versus 8%)
- Late re-bleeding rates: higher in coiled patients (2.9% vs 0.9% after clipping)
- Complete obliteration of aneurysm higher in clipping (81% versus 58% after coiling)
- Coiling also associated with lower risk of subsequent epilepsy and cognitive decline and decreased hospital length of stay
Other factors to consider
- Health care environment / equipment available
- Skill set and experience of the neurosurgeon / neurointerventionalist
Coiling generally prefered if
- Older Patients (>40)
- Low neck:dome ratio (thin neck)
- Significant comorbidities
- Basilar or posterior communicating artery aneurysms (hard to clip)
- Patient is on anticoagulation
Clipping generally preferred if
- Younger patients (<40) – less risk of recurrence later in life
- If a craniotomy is happening anyway e.g. for significant clot evacuation
- Multiple suitable aneurysms
Endovascular Adjuncts
- NOT USED if either coiling or clipping deemed feasible
- For ruptured, wide-necked aneurysms which can’t be clipped or coiled. stent-assisted coiling or flow diverting stents are an option
- For ruptured fusiform / blister aneurysms, low diverting stents are an option
- Anti-coagulation after flow-diverting stents can be problematic, particularly if an EVD is in situ
How are aneurysms clipped?
Simplified steps involved in clipping an aneurysm:
- Prepare the patient
- Perform a craniotomy
- Expose the aneurysm
- Deploy the clip
- Check the clip
- Close the craniotomy
Click below for a simple video describing one technique: