Clinical Case
You are still undecided on which ventilatory mode to select, so let’s try them all and figure out which one is the most appropriate.
At RNSH, we more often use Pressure Controlled modes, but lets first look at Volume Controlled modes and review some essential principles.
Volume Controlled (VC) Modes
With each breath, a set volume of gas is delivered at a set flow rate
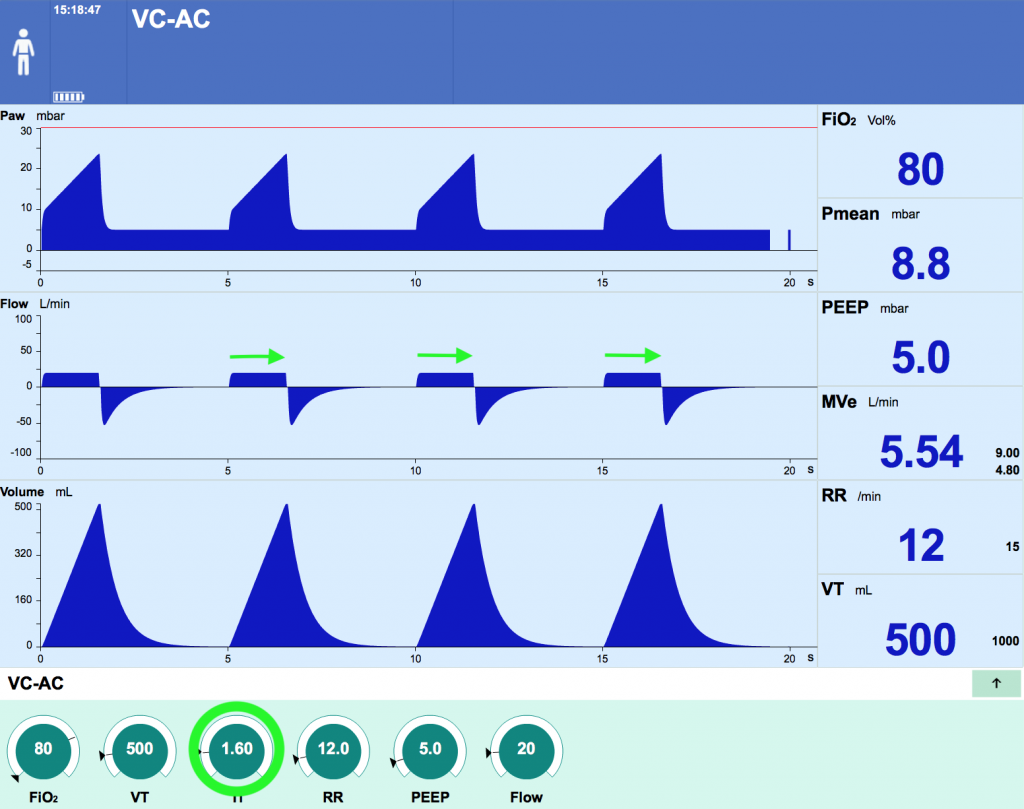
As you can is in the flow wave form, flow is constant throughout inspiration until the target volume is achieved which gives the characteristic “square waveform”
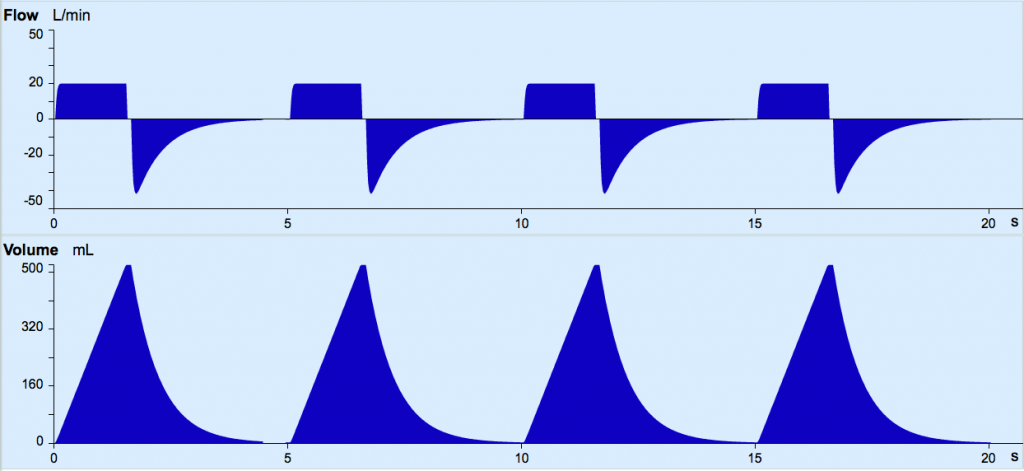
While we can adjust the Flow and Volume settings, the resultant pressure generated will depend on the patient’s lung mechanics and ventilator circuit; this is reflected as a variable pressure wave form.
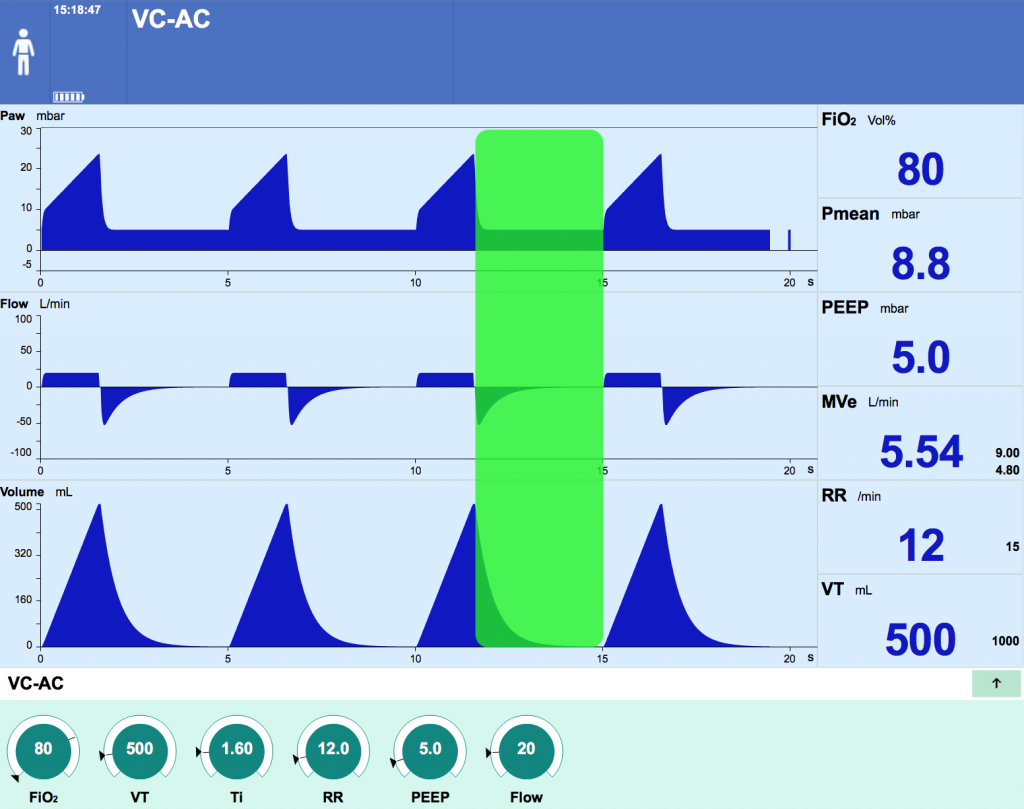
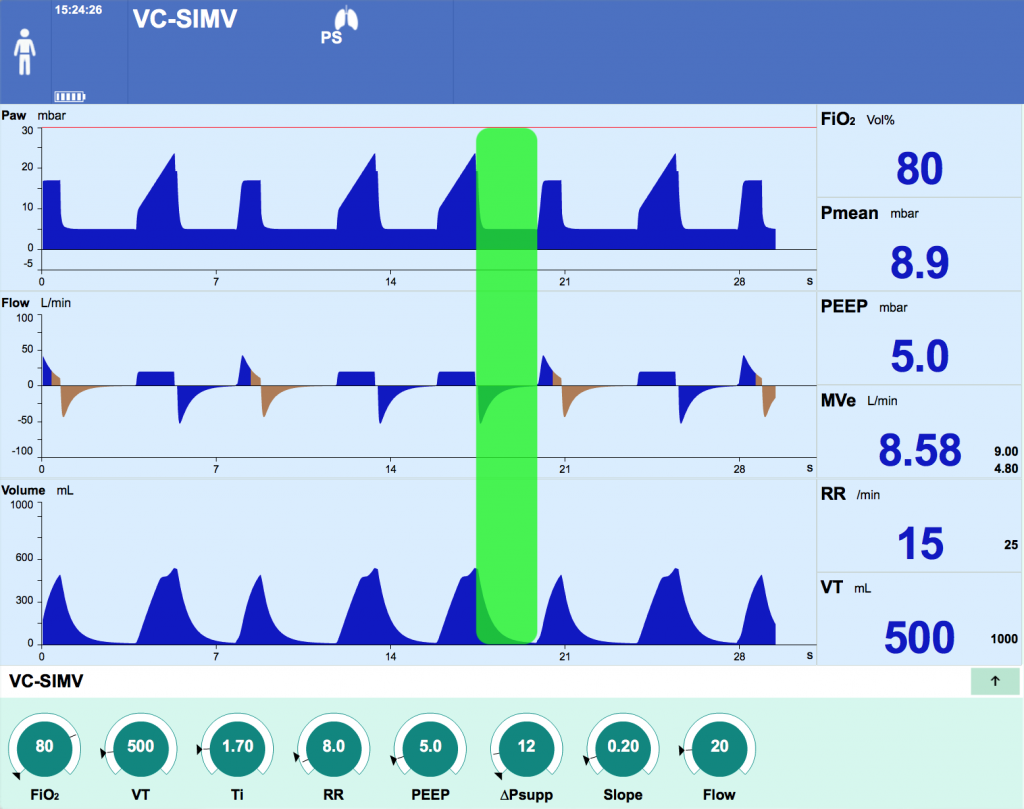
Having selected a target volume and flow rate, we will need to check 3 different values in the pressure waveform of a VC mode
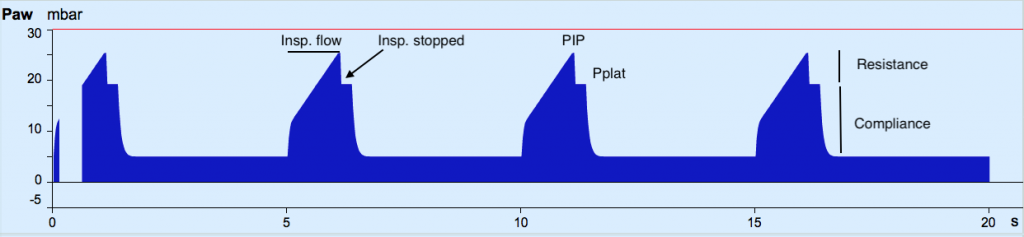
- Peak inspiratory pressure (PIP)
- The highest pressure reached during inspiration
- Principally affected by the system resistance (the tube in the diagram previously) and flow rates
- Increasing flow or volume will result in a higher peak pressure
- Plateau pressure (Pplat)
- The pressure within the lungs and circuit once inspiratory flow has stopped (just like during the inspiratory hold manoeuvre)
- As discussed, this approximates alveolar pressure
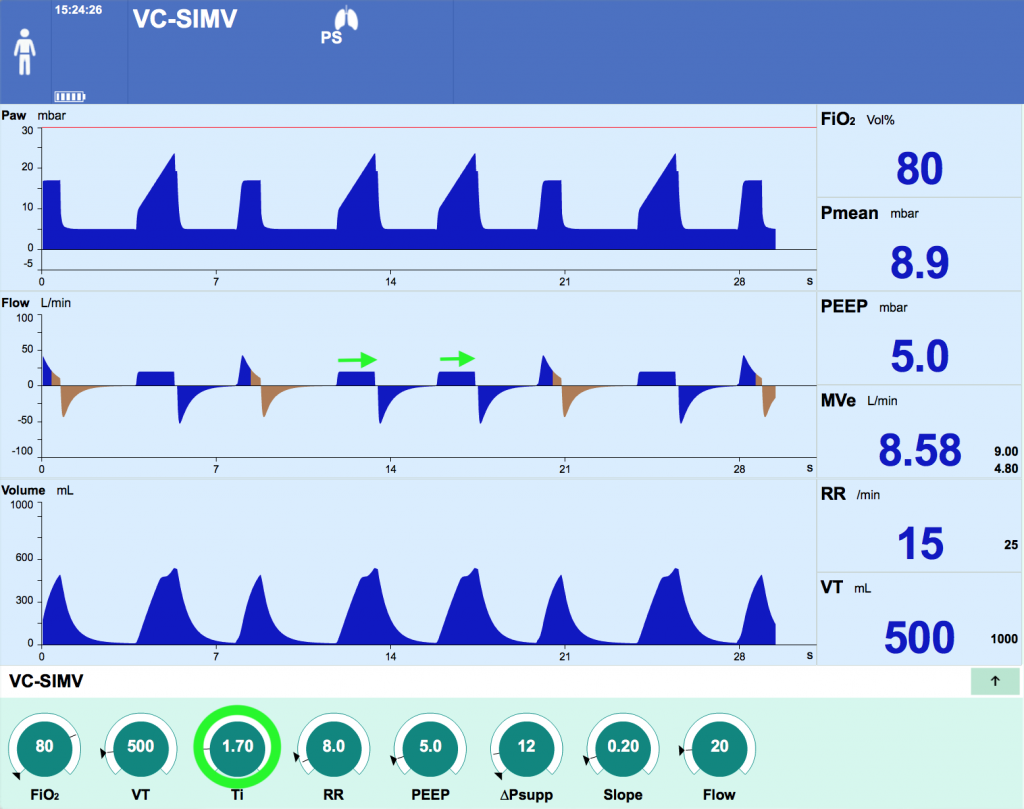
- Inspiratory pause time
- The time between reaching the preset VT and cycling into expiration during which there is no gas flow
- Dependent on the set inspiratory time (Ti) and flow rate
- Pause lengthens with increasing Ti and flow rates
- Volume Control – Assist Control (VC-AC)
- Volume Control – Synchronised intermittent mandatory ventilation (VC-SIMV)
- Continuous Mandatory Ventilation (CMV)
At RNSH, we rarely use VC-AC or CMV. Volume Controlled modes might be used where we want to guarantee a fixed tidal volume, for example in the neuro ICU where strict CO2 control might be required.
VC-SIMV is frequently used, but with auto-flow activated. Do you know how auto-flow changes the characteristics of the ventilation?
- This is a feature that is commonly used in modern ventilators when in a volume control mode. Almost all “Volume Controlled” modes used at RNSH use Auto-Flow
- Here, a target volume is set, however the inspiratory flow pattern changes from the constant flow typical of volume controlled ventilation to the flow seen in pressure controlled ventilation which we will discuss in due course (termed a ‘dynamic’ or ‘decelerating flow’ pattern).
- The ventilator measures system compliance and resistance and delivers the set tidal volume at the lowest possible inspiratory pressure.
- When auto-flow is activated, this mode should technically be considered a “Volume targeted, pressure controlled”, not “Volume Controlled” mode.
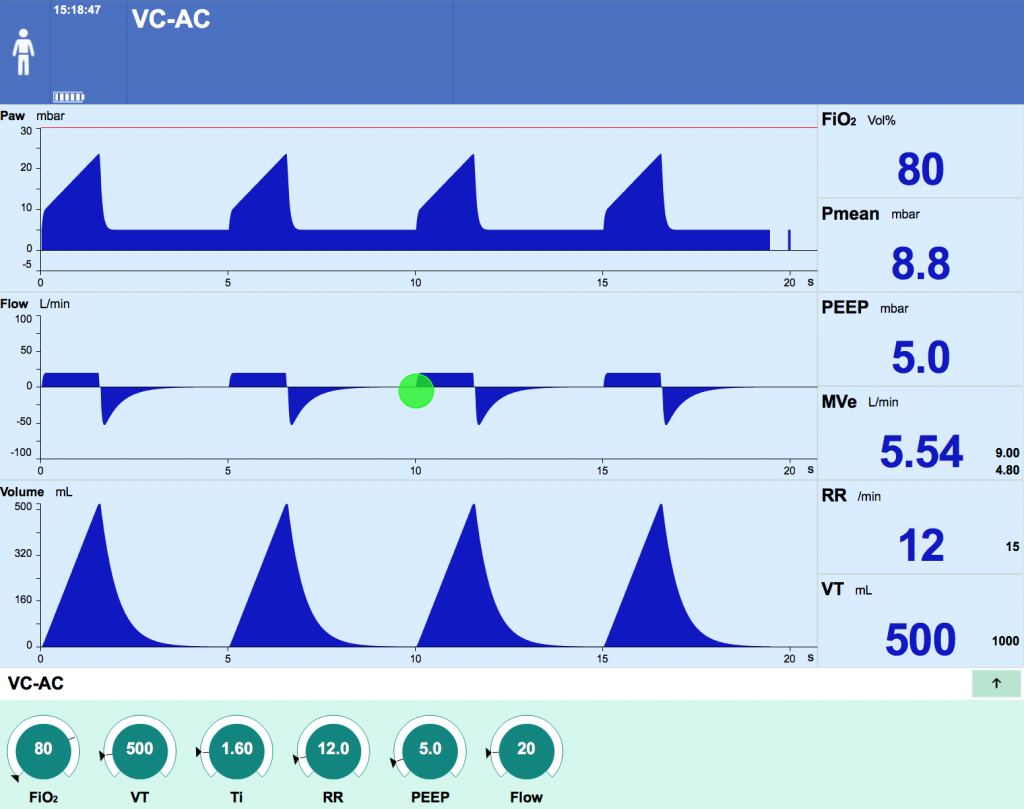
Volume Control – Assist Control (VC-AC)
This is a mode of VC ventilation where a mandatory rate is set, but the patient can trigger further VC breaths on top of the set rate. These extra breaths are termed ‘assist controlled breaths’ and are treated by the ventilator in exactly the same way the mandatory breaths are… unlike SIMV modes as we will discuss below.
The ventilator settings required are:
- FiO2
- Tidal Volume
- Respiratory Rate (you will have to set a RR, but it might be higher if patient triggers additional breaths)
- Flow
- Inspiratory time (Ti)
- PEEP
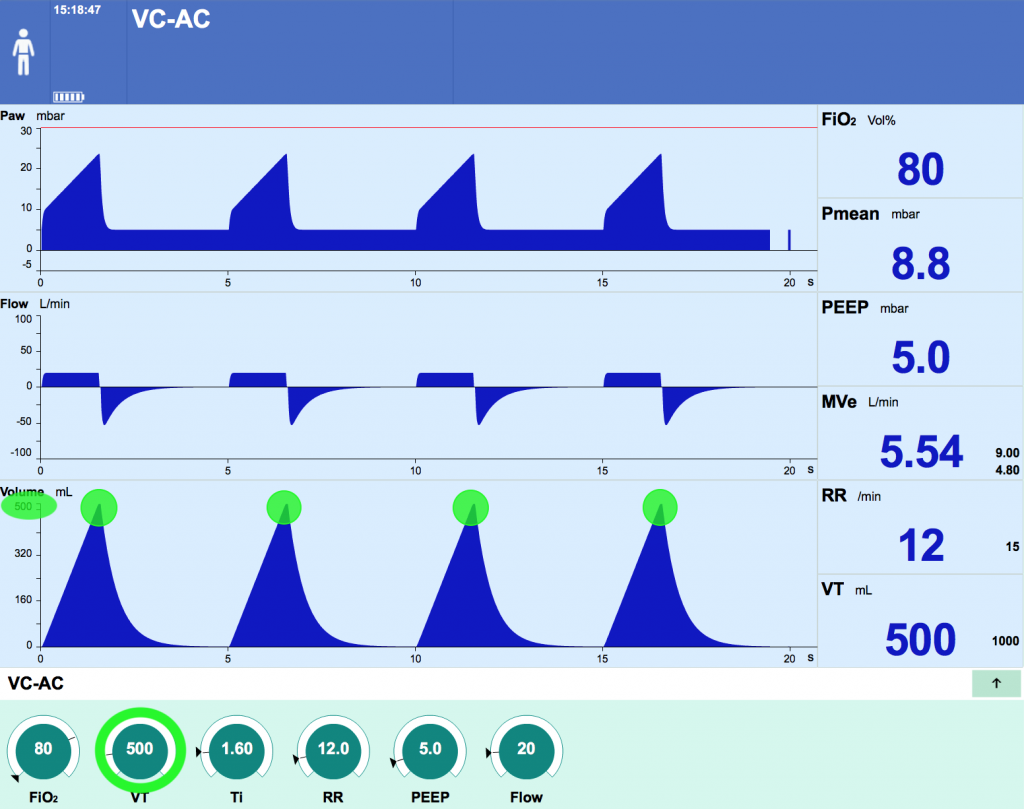
Press the different tabs to better understand the screen display.
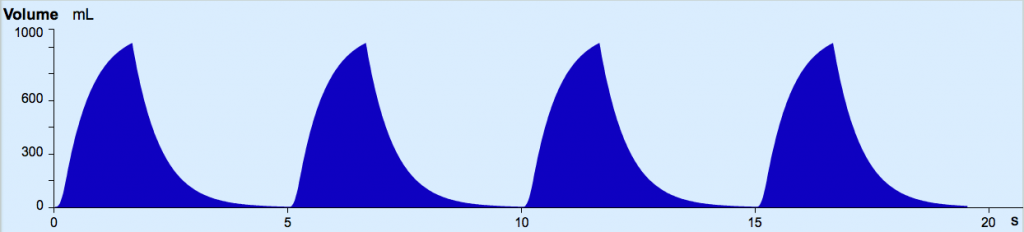
Lets imagine, you decide to try VC-AC on your patient as shown on the image above.
- There would be small negative deflection in flow
- There would be a small negative deflection in pressure
- The respiratory rate would exceed the set rate
- The curves would be different colour
- All of the above
(A) Inspiratory time (Ti)
(B) Expiratory time (Te)
(C) Expiratory flow
(D) Respiratory rate
Volume Control – Synchronised intermittent mandatory ventilation (VC-SIMV)
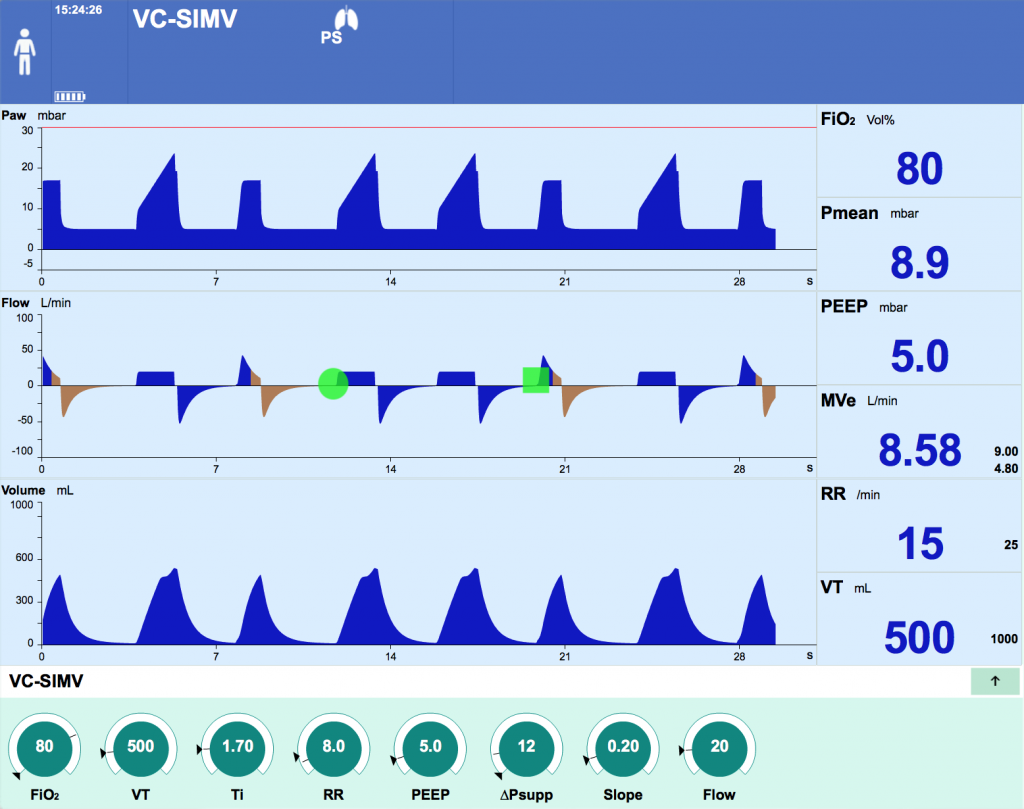
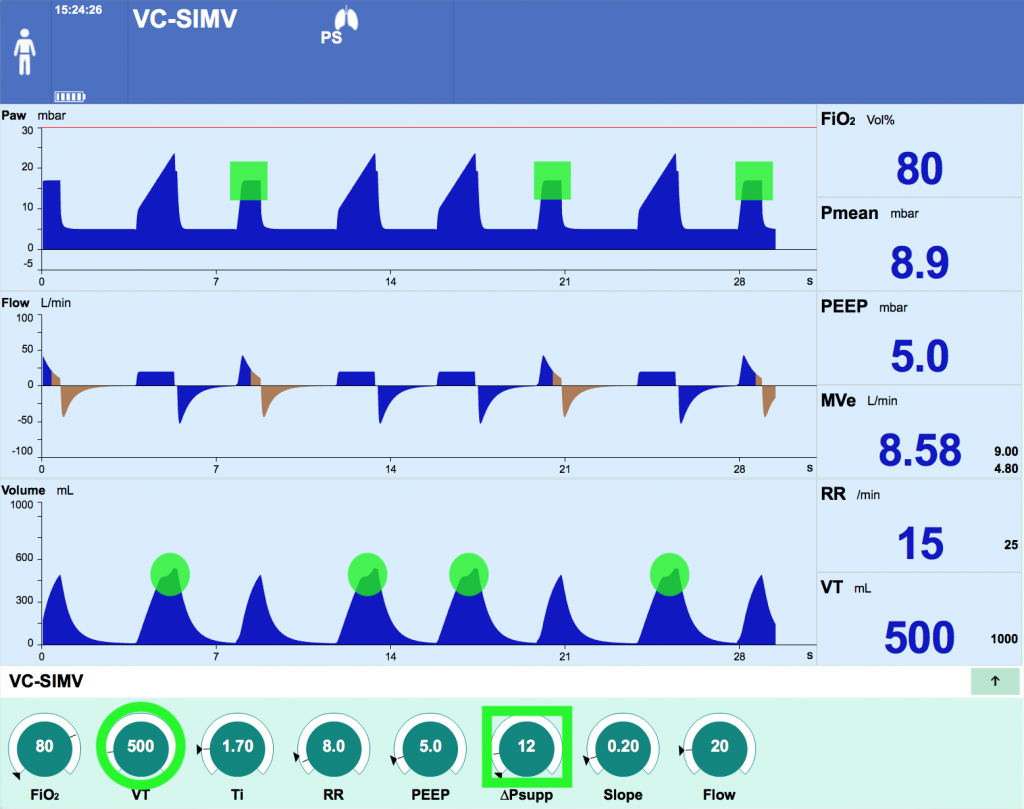
This mode allows two different types of breaths: VC breaths at a set rate (which may be ventilator or patient initiated) and Pressure Supported (PS) breaths for patient initiated breaths above the set mandatory rate.
Settings are required for
- General Settings: PEEP, FiO2
- VC breath settings (Tidal Volume, Ti, Respiratory Rate, Flow, Slope)
- Pressure Support (set as a pressure above PEEP) for the patient triggered PS breaths
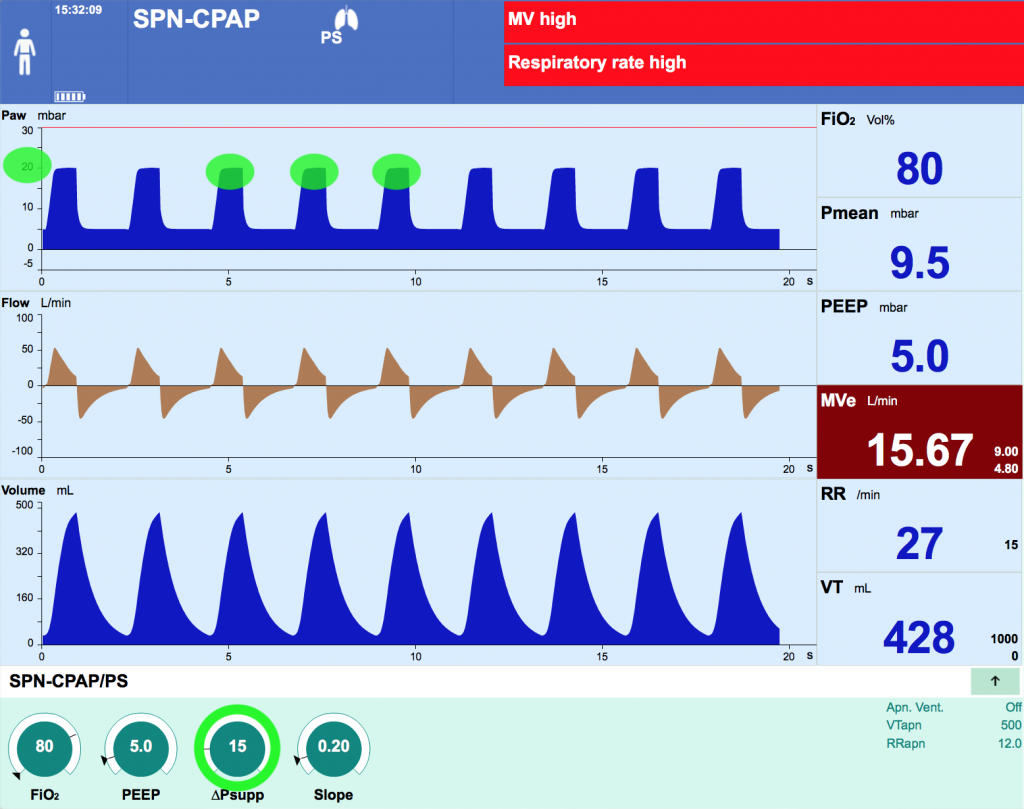
- Breaths may be triggered by the ventilator or the patient. The type of breath (VC or PS) varies depending on where in the breath cycle the respiratory effort is made.
- Patient’s inspiratory effort during the SIMV period triggers a mandatory full breath (round highlight). This has the same characteristics as an assist control breath
- Patient’s inspiratory effort during the spontaneous period triggers a PS breath (square highlight)
(A) After the patient has reached the number of mandatory breaths in 1 minute, all subsequent breaths are PS breaths
(B) It alternates evenly between pressure controlled and pressure supported until all pressure controlled breaths are delivered
(C) The minute is divided into equal intervals based on the set respiratory rate. In each of these windows, the first breath delivered is the mandatory breath and all subsequent breaths are PS breaths
(D) Based on current respiratory rate, the ventilator projects likely rate across the coming minute and calculates the need to deliver a mandatory breath based on this projected estimate
Continuous Mandatory Ventilation (CMV)
- This mode operates like VC-AC, except the patient can’t initiate (or trigger) their own breaths on top of the mandatory rate.
- RR and MV are always the same as what is set
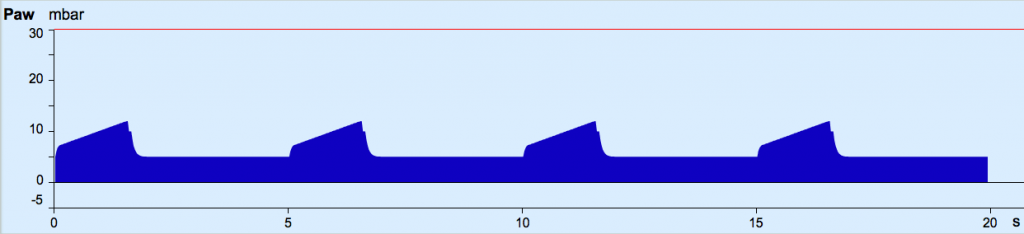
Pressure Controlled (PC) Modes
Gas flow is delivered at a variable rate in order to deliver a set inspiratory pressure (Pinsp). Pressure is constant during inspiration resulting in a square pressure waveform
- As outlined earlier, how quickly the ventilator achieves the set pressure is determined by the ‘slope’ setting
- Gas flow is dynamic in order to deliver a constant pressure: the flow waveform peaks at the start of inspiration and decelerates over time towards zero. Can you recall how the flow wave form differs in a volume control mode?
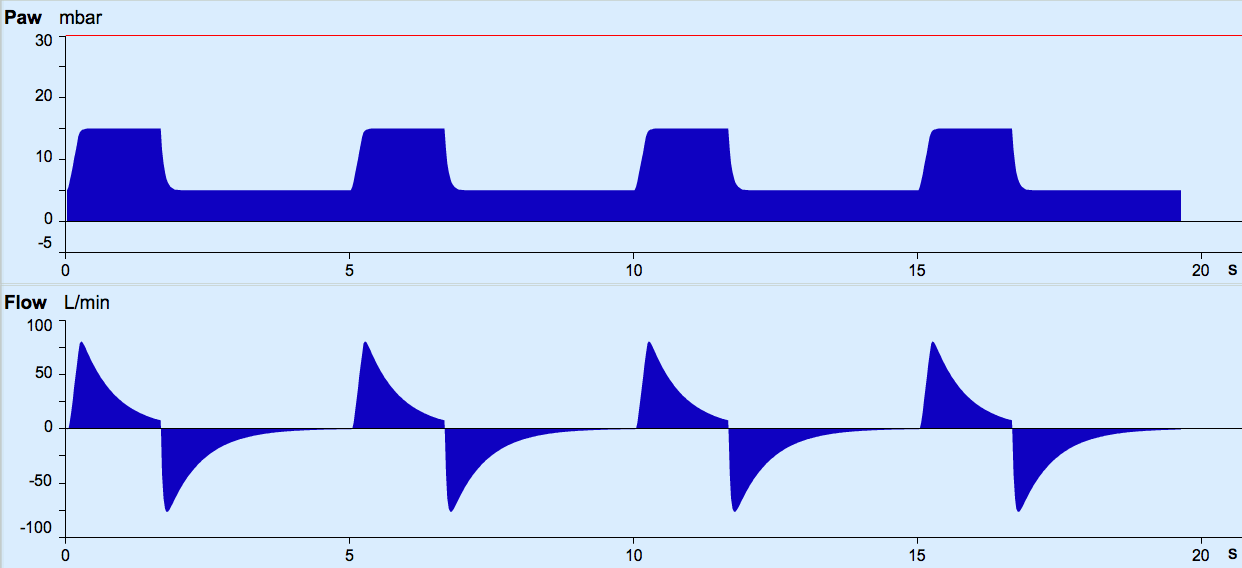
- The delivered tidal volume is determined by the pressure delivered (Pinsp) and the inspiratory time (Ti), as well as the patients lung mechanics (resistance and compliance)
- Increasing Pinsp on the ventilator will result in a higher VT
- Increasing lung resistance or reducing lung compliance will result in smaller VT
- PIP should not be set above 30cmH20 due to the risk of ventilator associated lung injury (VALI)
- Because the PIP can be specifically set, PC modes are often considered safest to avoid VALI.
- Pressure Control – Assist Control (PC-AC)
- Pressure Control – Synchronized Intermittent Mandatory Ventilation (PC-SIMV)
These modes are used frequently at RNSH, along with VC-SIMV with AutoFlow (which, as discussed earlier, may too be considered a pressure controlled mode, or “volume targeted, pressure controlled”).
These modes tend to more comfortable for patients, offer better synchrony, and offer the safety of strict control of Peak Inspiratory Pressures, and thus prevention of ventilator associated lung injury.
Pressure Control – Assist Control (PC-AC)
This mode of ventilation is often used in hypoxic patients, and is often the “Go-to” mode when patients are difficult to ventilate.
Each breath, whether patient triggered or mandatory, is a pressure controlled – delivered as a set pressure, for a set time. Patient triggered breaths are termed “assist controlled” breaths as they differ significantly to patient triggered “pressure supported” breaths in SIMV modes.
Ventilator settings required:
- FiO2
- Respiratory Rate
- Inspiratory time (Ti)
- Inspiratory Pressure (Pinsp)
- PEEP
(A) PInsp-PPlat/TVol
(B) PPlat-PEEP/TVol
(C) PPlat-PInsp/Tvol
(D) You can’t; can only measure dynamic compliance
Pressure Control – Synchronised Intermittent Mandatory Ventilation (PC-SIMV)
This is another SIMV mode. Here, the mandatory breaths are Pressure Controlled breaths (set as a PInsp and Ti) which are interspersed with Pressure Support (PS) breaths, just as for VC-SIMV described above.
At RNSH, we may use PC-SIMV, but more commonly use VC-SIMV with Auto-flow as described above.
Spontaneous Modes
In contrast to the mandatory modes described above, every breath in a spontaneous mode of ventilation is patient triggered. These are often referred to as ‘supported breaths’.
- Pressure Support
- CPAP (Continuous Positive Airway Pressure)
Pressure Support (PS)
This is a purely spontaneous mode- each breath triggered by the patient is supported by a set level of positive pressure support.
- Ventilator settings required
- FiO2
- PEEP
- PS
- Slope
You will have noted while you were trying VC-SIMV above, your patient’s paralysis has worn off and that he is triggering some breaths.
So lets see what happens when we trial him on PS.
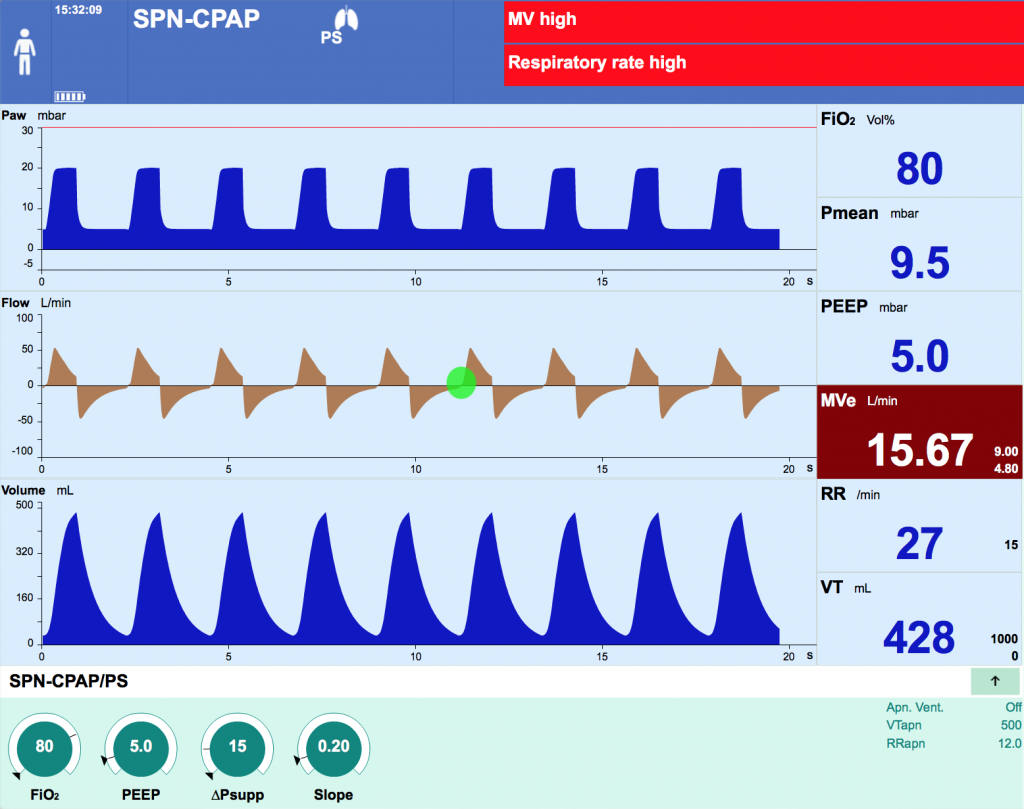
Press the different tabs to better understand the screen display.
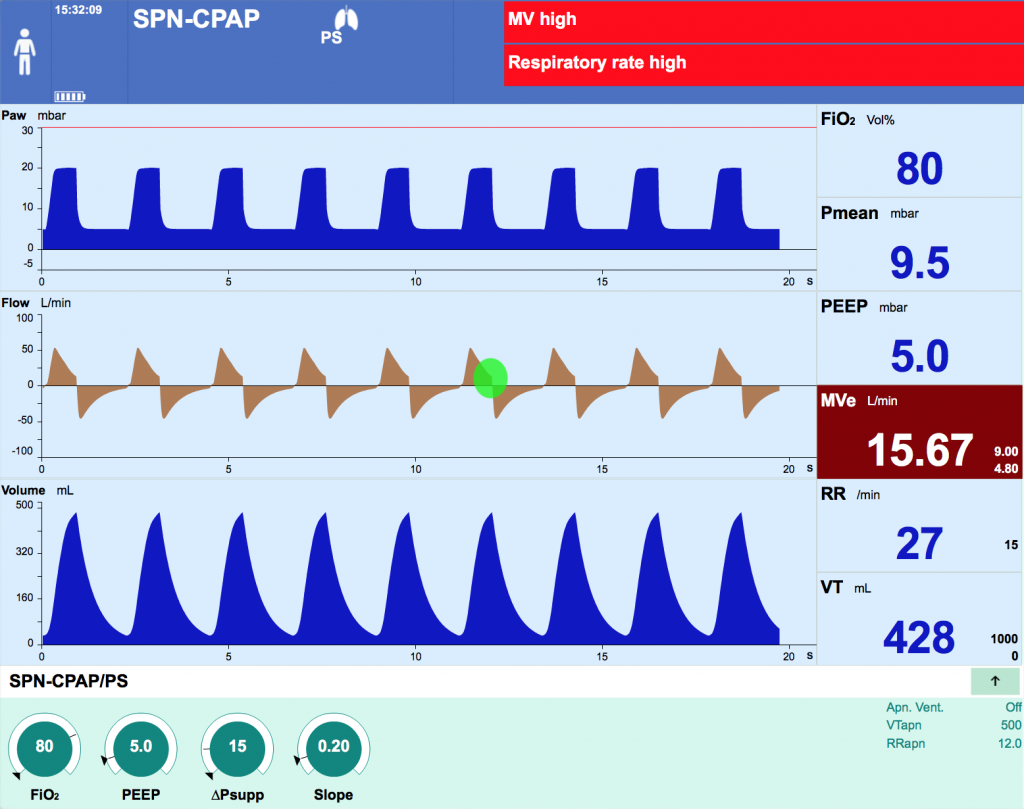
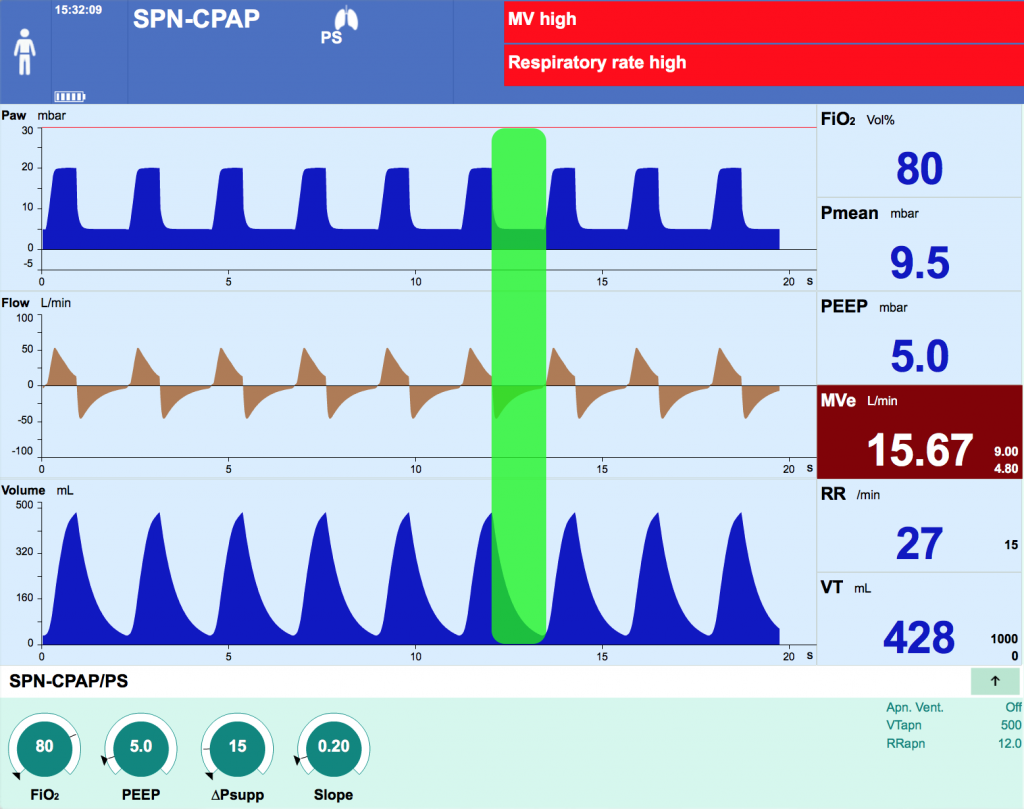
- A supported breath is triggered when the ventilator detects that patient effort has generated a change in flow or pressure within the circuit
- In this case you set it as a flow trigger of 3L/min and your patient easily triggers his breaths (The flow curve is a beige colour when the breath is patient-triggered instead of blue)
- You should note that apnoea ventilation back-up setting is off in this case.…sometimes this is used as a backup.
- Breaths are limited by the amount of pressure support (PS) set above PEEP
- Total pressure = PS + PEEP
- PS set at 15 cmH2O and PEEP at 5 cmH2O = total pressure 20 cmH2O
- The tidal volume (TV) generated for the set PS will be dependent on lung mechanics and compliance
- The higher the PS, the greater the TV for each individual patient
- TV can be dynamic, for example in asthma where the degree of bronchospasm may change.
Continuous Positive Airway Pressure (CPAP)
“CPAP” is often used to describe low levels of Pressure Support (eg 5cmH20 Pressure Support on 5cmH2O of PEEP). Strictly, this is not correct.
In true CPAP mode no PS is set, just PEEP, and TV is purely dependent on patient effort.