Clinical Case
Your ventilator has been set up and checked, but its still not quite ready to go… You will now have to enter your ventilator settings.
During mechanical ventilation, there are four things that need to be considered for every breath:
- Inspiratory Trigger
- Limit
- Cycle
- Slope
- Expiration
Lets look at each of these in detail
Inspiratory Trigger
This is how the ventilator decides when to deliver a breath. Breaths can be either machine or patient triggered.
These are independent of patient respiratory effort and are initiated at a set time interval according to the set respiratory rate
Here, the ventilator initiates the breath when the patient’s inspiratory effort causes a change in either flow or pressure within the ventilator circuit.
The set trigger sensitivity determines how easy it is for the patient to initiate (trigger) the breath. The lower the trigger threshold setting, the easier it is for a breath to be triggered and vice versa.
Setting the trigger threshold too low risks ‘auto-triggering’ where a breath is triggered without patient inspiratory effort such as by hiccups or cardiac oscillations.
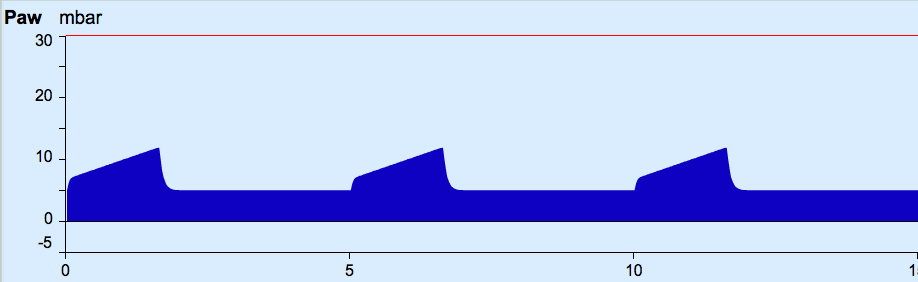
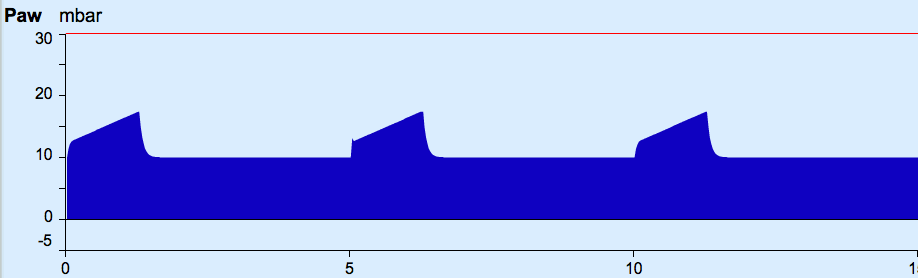
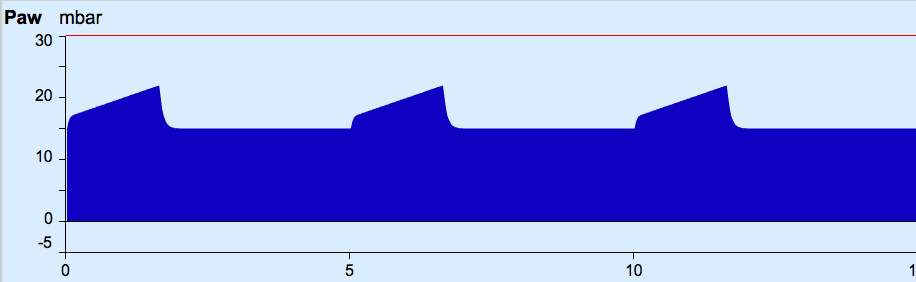
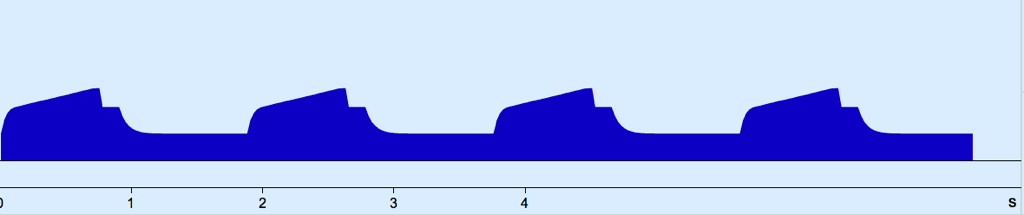
(A) Pressure Supported mode, 1L/min flow as trigger
(B) Pressure Supported mode, 3L/min flow as trigger
(C) Pressure Supported mode, pressure as trigger
(D) Pressure Controlled mode (thus, time as trigger)
Limit
The ‘limit’, also known as the ‘control variable’, is the value we set to determine the size of each breath. When the ‘limit’ is reached gas flow into the lungs stops.
Gas is then held until expiration begins.
‘Limit’ should not be confused with the breath ‘Cycle’ which is described below.
(A) Pressure controlled ventilation
(B) Volume controlled ventilation
Cycle
‘Cycling’ refers the point at which the ventilator switches from inspiration to expiration.
The ventilator cycle may be triggered by time, flow or pressure.
- Time cycled: expiration commences when the set inspiratory time is complete
- Flow cycled: once the inspiratory flow rate falls to a set percentage (eg 25%) of peak inspiratory flow the expiratory valve opens and allows commencement of expiration
- Pressure cycled: Once inspiratory pressure reaches the set pressure limit (eg 35cmH2O), the expiratory valve opens. This is usually intended as a safety feature as it frequently occurs with acute problems rather than the completion of the intended breath.
Slope
‘Slope’ refers to the time taken at beginning of inspiration for the ventilator to get to peak flow or peak pressure.
The usual setting is around 0.2 seconds.
Increasing this rate (ie. by reducing the set time), may increase peak pressure. Conversely, too slow (ie. by increasing the set time) can lead to inadequate supply to meet demand, and associated air hunger and increased work of breathing.
Expiration
Expiration remains a passive process, driven by the elastic recoil of the lung and chest wall.
The only features controlled in expiration are the level of positive end expiratory pressure (PEEP) and the time allowed for expiration, determined by the I:E Ratio.
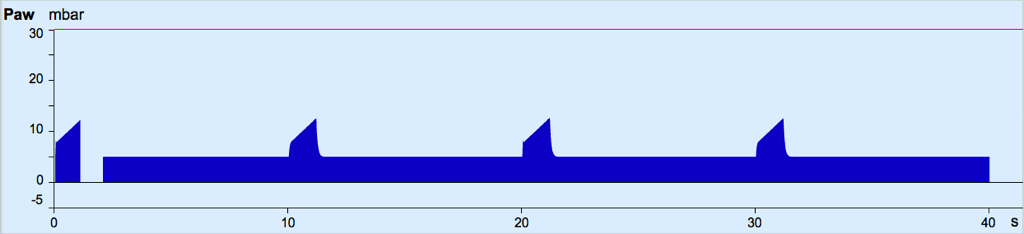
Positive end expiratory pressure (PEEP)
PEEP refers to the positive airway pressure is maintained above atmospheric pressure throughout expiration. When using a non-invasive ventilator, this is known as EPAP: Expiratory Positive Airway Pressure.
Explore the impact of varying the PEEP on a Volume Controlled Mode below. Note that in this mode, the peak inspiratory pressures increase with PEEP, along with the mean airway pressures.
It is important to remember that while altering PEEP may increase the peak inspiratory pressures (PIP) in some ventilator modes, in other modes the PIP may be fixed so that increasing the PEEP reduces the driving pressure (the difference between PIP and PEEP) for each breath .
I:E ratio
The length of time allowed for expiration is determined by the I:E ratio and the respiratory rate. The I:E is the ratio of the inspiratory time (Ti) to the expiratory time (TE)
The expiratory time is determined by the set inspiratory time (Ti) and the respiratory rate, as outlined below
- Respiratory rate determines the total length of inspiration/expiration cycle.
- Ti is set on the ventilator in seconds
- The rest of the breath is therefore expiration
Thus, if the Ti remains fixed, with increasing RR, the expiration phase must shorten, and the I:E ratio approaches 1:1 (or an inverse ratio).
For example:
10 breaths per minute gives 6 seconds per breath
if Ti is set at 1.5s
expiratory time will therefore be 4.5s
I : E = 1 : 3
The I:E ratio can be altered for specific conditions, for example
- Longer Ti (and thus I:E ratio approaching 1:1 (or larger)) may be used in hypoxia
- Longer TE ((and thus smaller I:E ratio) may be used in obstructive lung disease to prevent gas trapping
The Ti may also be increased an inspiratory pause which is a period during inspiration during which no gas flow. This may increase mean airway pressure (and oxygenation) but reduces the time for expiration and thus CO2 clearance.