Clinical Case
The repeat ABG you ordered came back and looks improved and the rest of the night was uneventful.
In the morning, the team decides that given the patient is oxygenating better on FiO2 60%, its time to assess if they can move the patient towards a gradual weaning from mechanical ventilation. They start by lowering sedation while on VC-SIMV with a pressure support of 12cmH2O, but they are rapidly concerned by the curves they see and the patient looks uncomfortable.
Ventilator Dyssynchrony
Looking at the ventilator wave-forms below, lets see if we can figure out what’s driving this patient’s ventilator dyssynchrony…
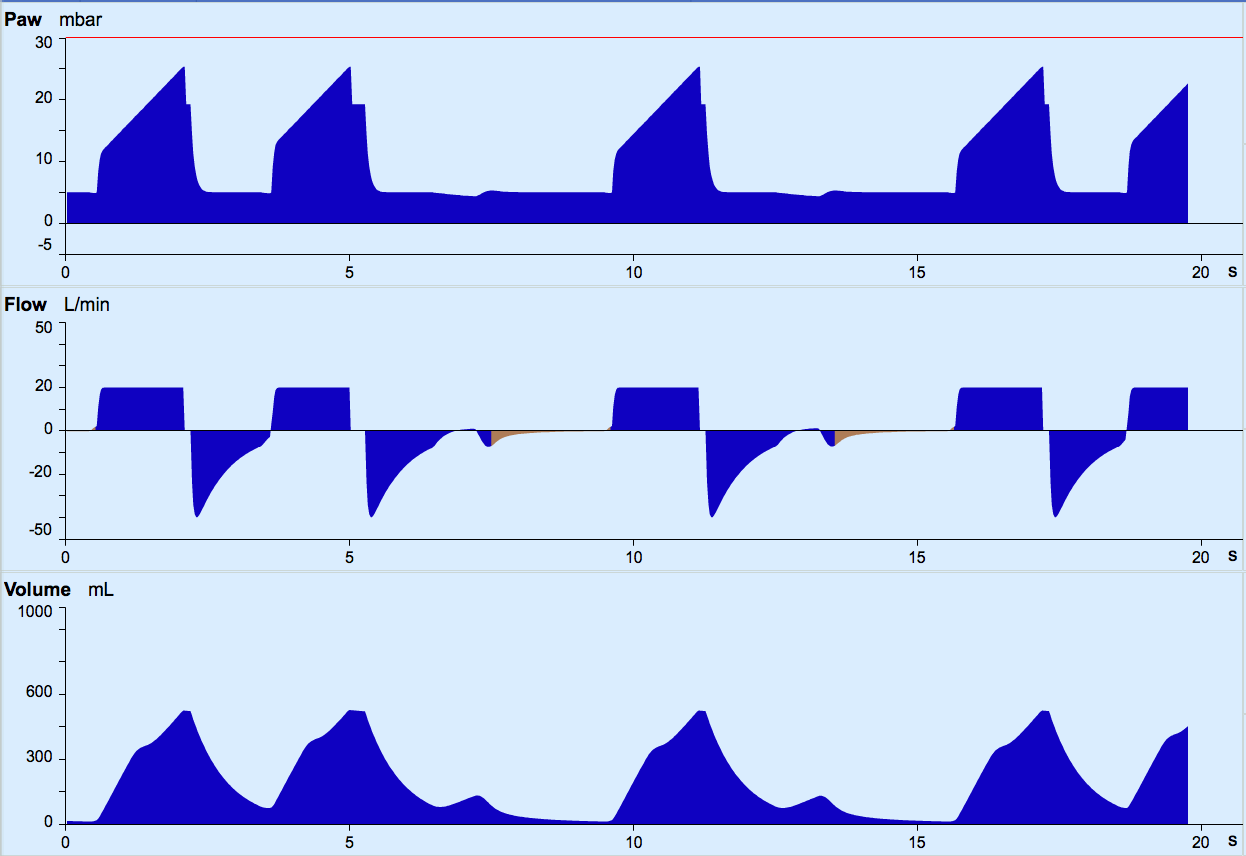
Dyssynchrony often occurs when the ventilator settings don’t match the patient’s requirements. It can cause
- Increased work of breathing and muscle fatigue
- Increased oxygen requirements
While management often requires increased sedation (which may prolong the duration of ventilation), in the first instance, an attempt should be made to adjustment ventilator settings or transition to a more comfortable mode; many argue that PC modes, or VC modes with auto-flow are more comfortable and less likely to induce dyssynchrony.
Types of Dyssynchrony
The trigger may be inappropriate in a mandatory mode with no ability to trigger spontaneous breaths (VERY uncomfortable!) or in spontaneous mode, as outlined below:
Trigger set too high
A weak patient will be unable to initiate a spontaneous breath as they won’t sufficiently change the flow or pressure in the circuit
Trigger set too low
Other actions for example hiccups will trigger a breath
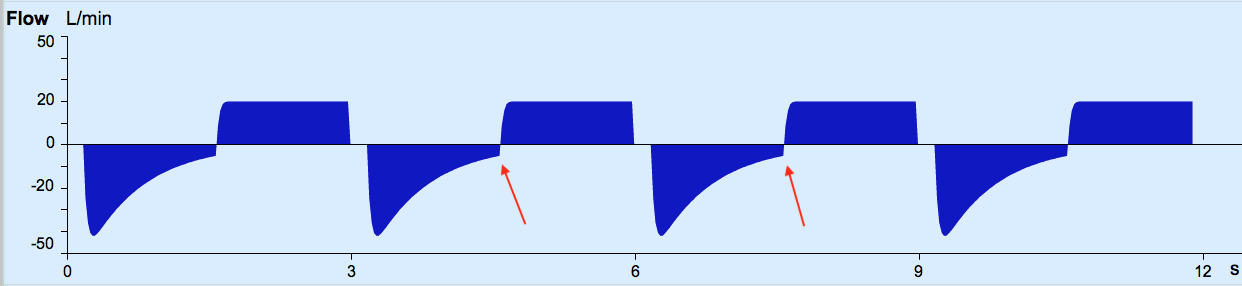
Flow set too low
results in insufficient TV being delivered and the patient may appear to be sucking or gasping
Flow set too high
results in either an excessively large breath or the patient tries to initiate expiration early and works against the ventilator
Ti set too short
Prematurely ends inspiration and can result in inadequate TV
Patient discomfort as still trying to inspire when expiration begins
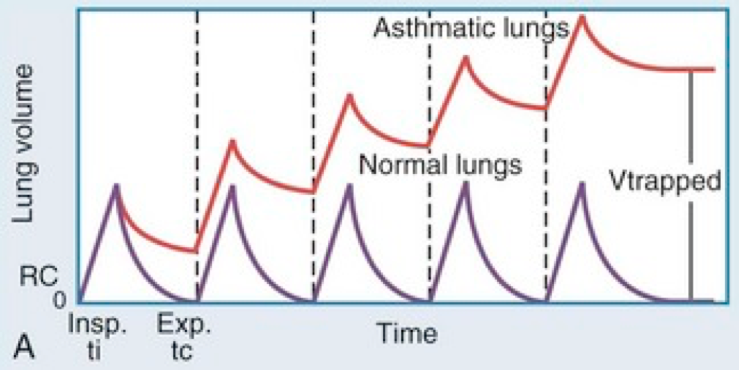
Ti set too long
Can result in excessive TV
In obstructive lung disease the resulting lack of expiratory time can result in gas trapping
Intrinsic PEEP / Gas Trapping
Intrinsic PEEP is also known as Auto PEEP or PEEPi
- Develops when there is an inability to exhale the complete breath
- Seen on Flow curve: patient still exhaling when next breath starts
- Contributory factors include
- Increased expiratory resistance
- Bronchospasm from Asthma/COPD
- Circuit factors
- HMEs
- Kinked ETT
- Too short expiratory time
- when the Ti is set too high for the set RR
- A combination of both
- Increased expiratory resistance
- Results in gas being trapped in the lungs
- Increased pressure for the given volume can cause barotrauma
- Trapped gas increases intra-thoracic pressure which reduces venous return, preload and cardiac output causing hypotension
- The amount of gas that is unable to be expired progressively increases with each breath and can result in dynamic hyperinflation. Eventually it becomes difficult to inhale at all and tidal volumes and compliance progressively fall, with hypercarbia and resulting cardiorespiratory collapse (image 8.3.2)
- Measured using end expiratory hold in a sedated/paralyzed patient
- Occlusion of the expiratory flow for 3-5 seconds allows the pressures within the airways to equilibrate
- The resulting measure is called a static PEEP or total PEEP and is in fact the alveolar pressure at end of expiration
PEEPi is the “extra PEEP” over the PEEP you had set.
PEEPtot = PEEPset + PEEPi
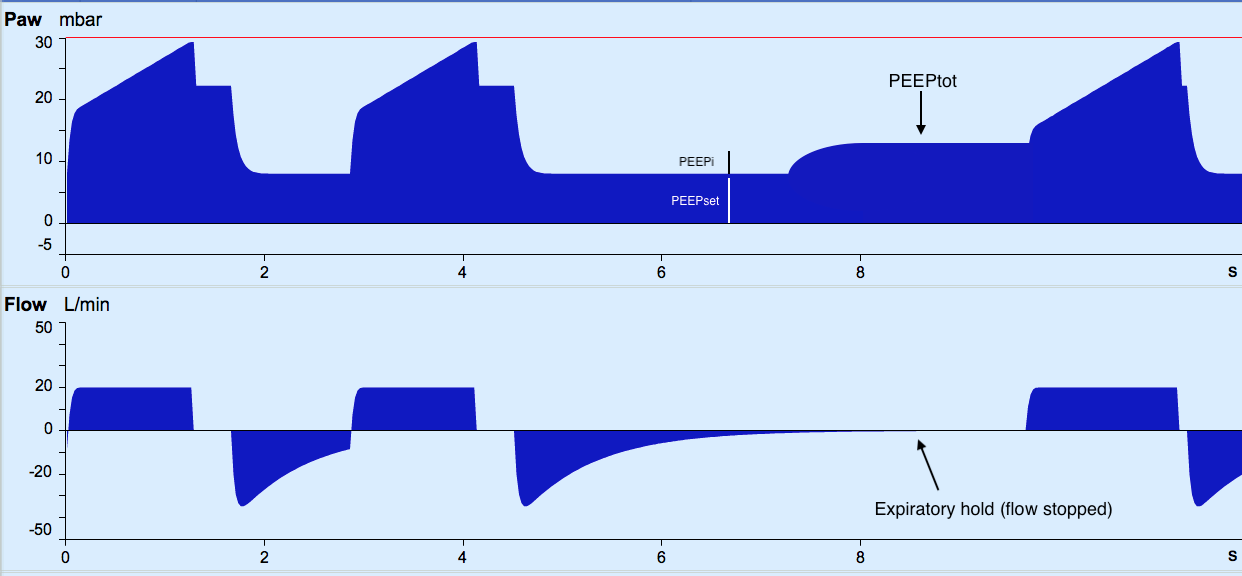
You last set PEEP at 10cmH2O and PEEP total is measured at 14 cmH2O during the expiratory hold.

