Coma comes from the Greek ‘‘deep sleep or trance’’
Coma is characterized by the absence of
- Arousal (wakefulness, vigilance) AND
- Awareness of self and environment
- Lasting for > 1 hour
PATHOPHYSIOLOGY OF CONSCIOUSNESS
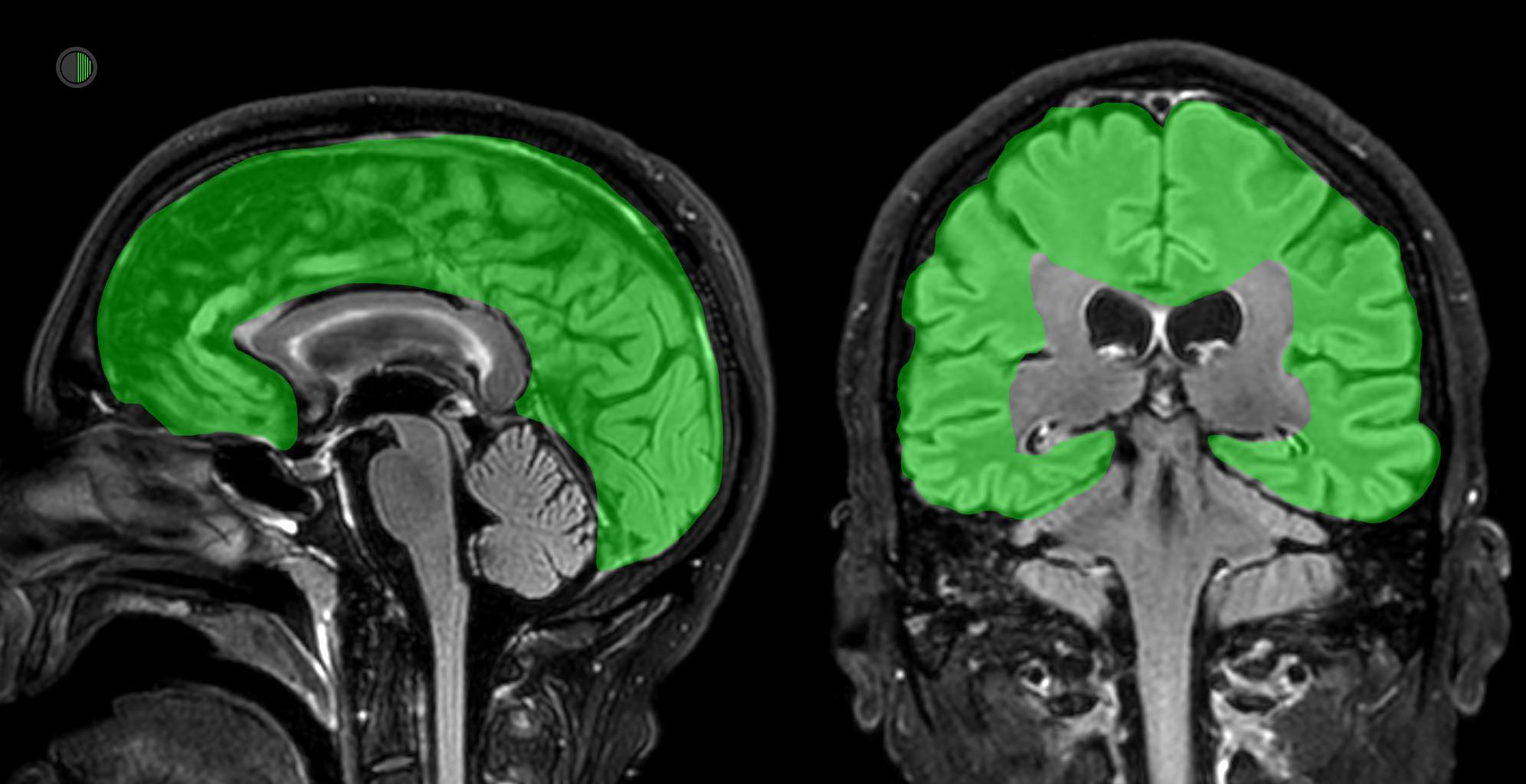
Normal consciousness depends on the interaction between the two cerebral hemispheres and the ascending arousal system (AKA Reticular Activating System (RAS) in the upper brain stem.
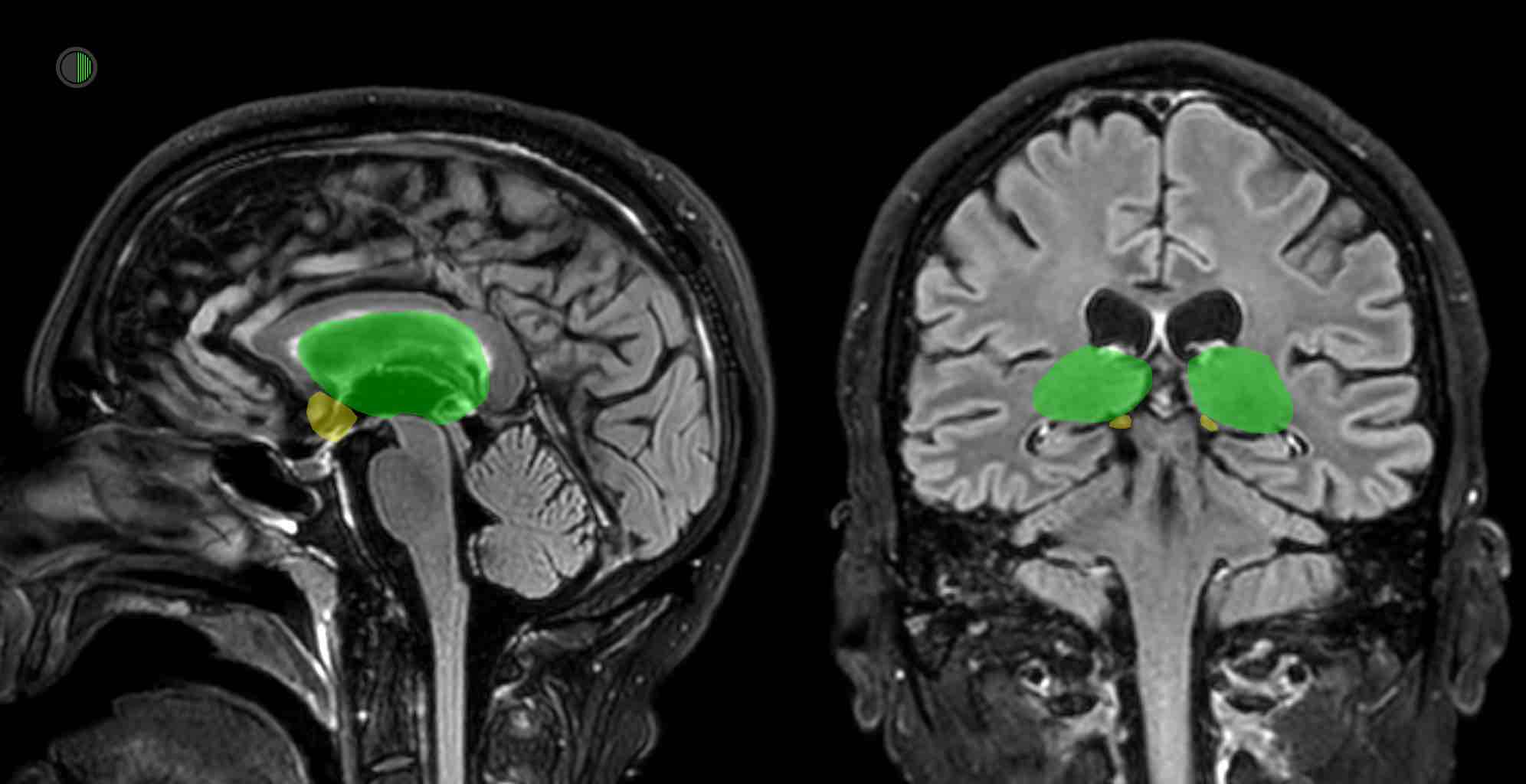
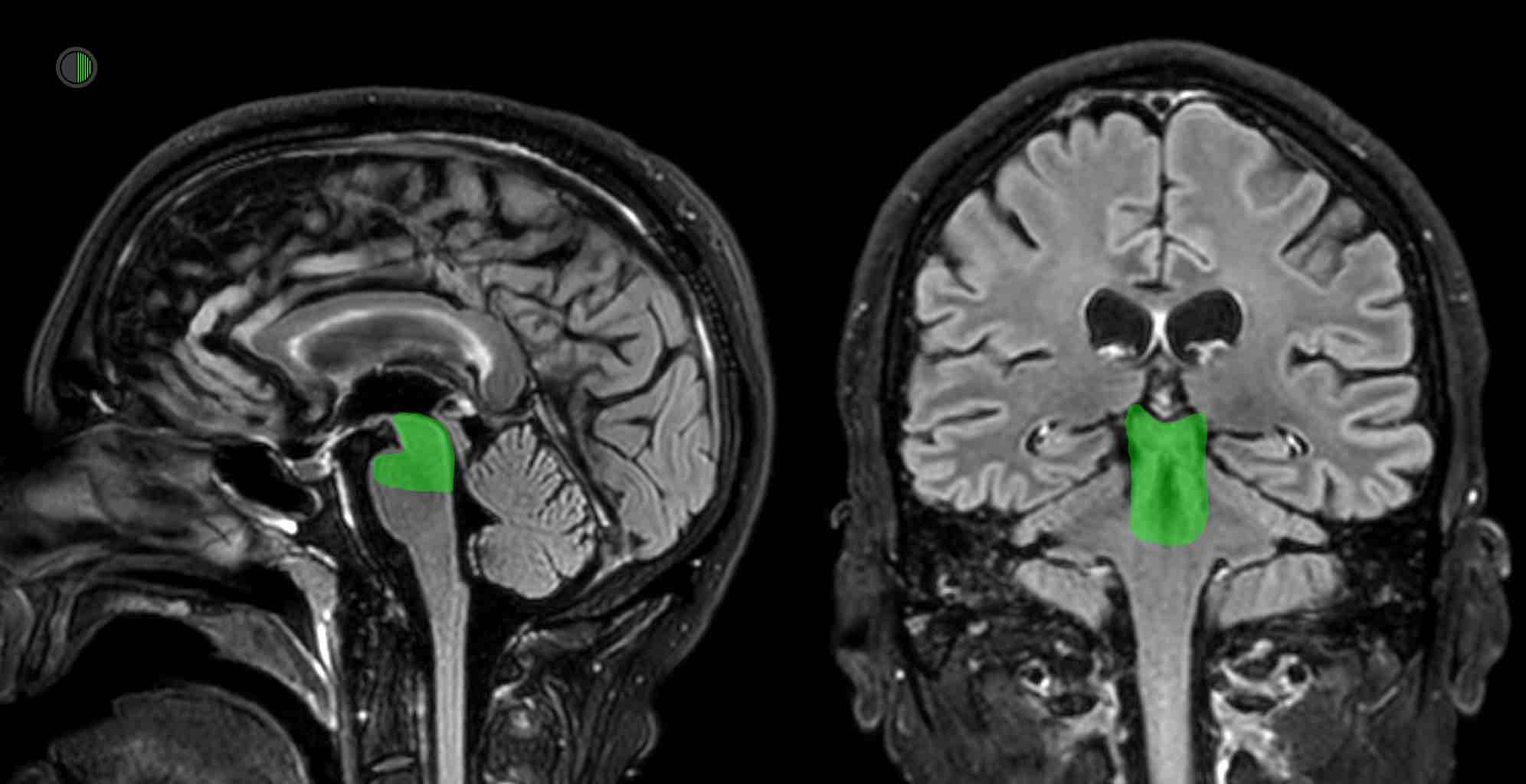
The ascending arousal system is an extensive network of nuclei and interconnecting fibres in the upper pons, midbrain, and posterior diencephalon.
This system originates in the tegmentum of the upper pons and midbrain, projects to the hypothalamus and bilateral thalami, and subsequently diverges widely throughout both cortices, many pathways going via the basal forebrain and the prefrontal cortex.
Consciousness is not focally represented in the cerebral hemispheres and in many ways is related to the mass of functioning cortex, but relies on a few key areas:
> Ascending arousal system
> Thalami
> Basal ganglia MORE
> Posterior hypothalamus
> Basal forebrain
> Midbrain tegmentum
Of course consciousness is more complicated than the gross anatomy.
See here for a brief summary of theories of consciousness
WHAT CAUSES STRUCTURAL COMA?
Three types of structural coma:
> Bilateral widespread cortical injury
> Bilateral diencephalon (thalamus, hypothalamus) injury
> Ascending arousal system injury
The thalamus plays a key role in wakefulness and consciousness
Any lesion here sufficiently large or in the wrong spot may cause unconsciousness, particularly the posterior intralaminar thalamic nuclei
CAUSES
> CVA: “Tip of the basilar syndrome” can cause bilateral thalamic infarction
> ICH: Thalamic haemorrhage
> Hypoxic brain injury (thalamus one of the more vulnerable regions)
> Tumours e.g. injuring hypothalamus
> Inflammatory lesions e.g Bechet’s syndrome
The midbrain and upper pons are critical to consciousness
Specifically the paramedian tegmental zone immediately ventral to the periaqueductal gray matter, from the caudal diencephalon through to the the rostral pons
CAUSES
> CVA: Basilar artery occlusion
> ICH: Upper pontine haemorrhage
> Compression causing ischaemia: e.g. from posterior fossa ICH
CLASSIFICATION
Many ways this can be done as so many disorders end up with unconsciousness.
The classic Plum & Posner classification uses the location of the aetiology as the structure:
- Structural
- Metabolic
- Mimics (e.g. Locked-in Syndrome, aphasia, abulia, catatonia)
In one study, the commonest causes of coma where neurologists get consulted because the initial cause wasn’t clear and imaging hasn’t happened yet were:
- Tox syndromes
- ICH
- SDH
- Brainstem stroke
By adding the presence of focal neurological signs and meningism to the categorization, it is perhaps more practically useful:
Mass lesions
> ICH
> SDH
> EDH
> Brain abscess
> Brain tumour (metastatic > primary)
Stroke (AIS)
> Thrombotic
> Embolic
> Venous obstruction
CNS Infection
> Meningitis
> Encephalitis
Subarachnoid Haemorrhage
> Aneurysmal
> Traumatic
[M] Metabolic
> Hyponatraemia (usually sudden, below 110 mmol/L) REF
> Hypernatraemia (usually > 160 mmol/L) REF
> Hypoglycaemia (< c. 2.2 mmol/L) REF
> Hyperglycaemia (> c. 50 mmol/L) REF
> Hypoxia
> Hypercapnoea (PaCO2 > c.80 mmHg, depending on normal)
> Hypo / hyperthermia
> Hyper / hypo-osmolar
> Hypercalcaemia
[E] Endocrine
> Myxoedema crisis
> Hypopituitarism
[S] Seizures
> Convulsive
> Non-convulsive
[O] Organ Failure
> Hepatic encephalopathy
> Renal uraemia
[T] Toxins
> Narcotics
> Alcohol
> Psychotropics
> Carbon monoxide
> Loads of others