Clinical Case
Based on the information gathered so far, you know your patient’s lung mechanics are as follow:
However, 4h post-admission to ICU, you are called by the bedside as your colleague is concerned…
Hypoxia
Walk through the break-down tree to figure out how!
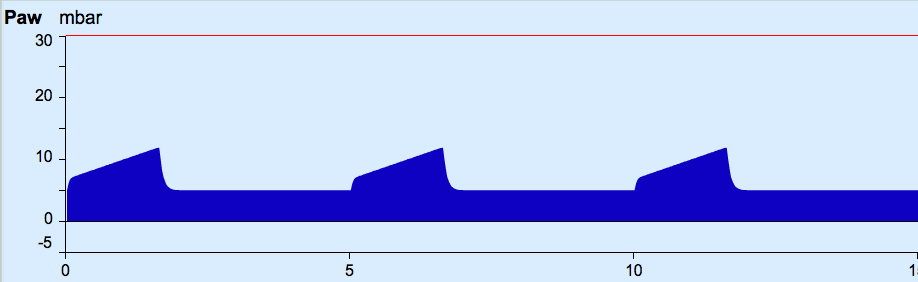
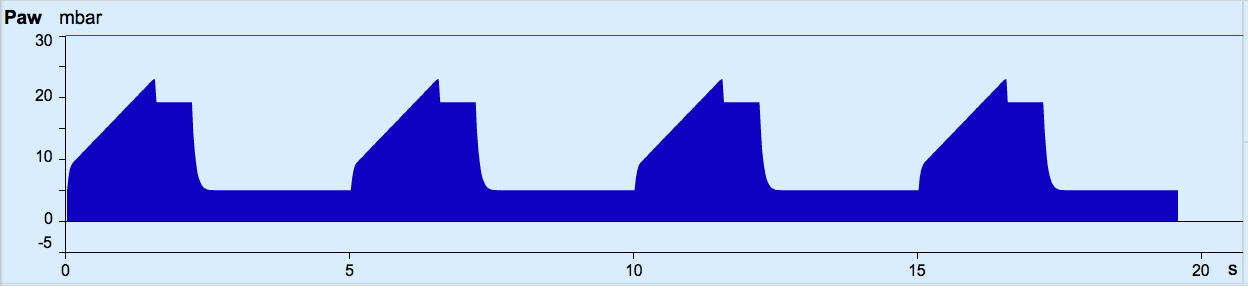
- Increases the mean pressure during the overall respiratory cycle (in some modes, it may not increase the inspiratory pressure)
- May improve oxygenation by recruiting collapsed alveoli and decreasing shunt
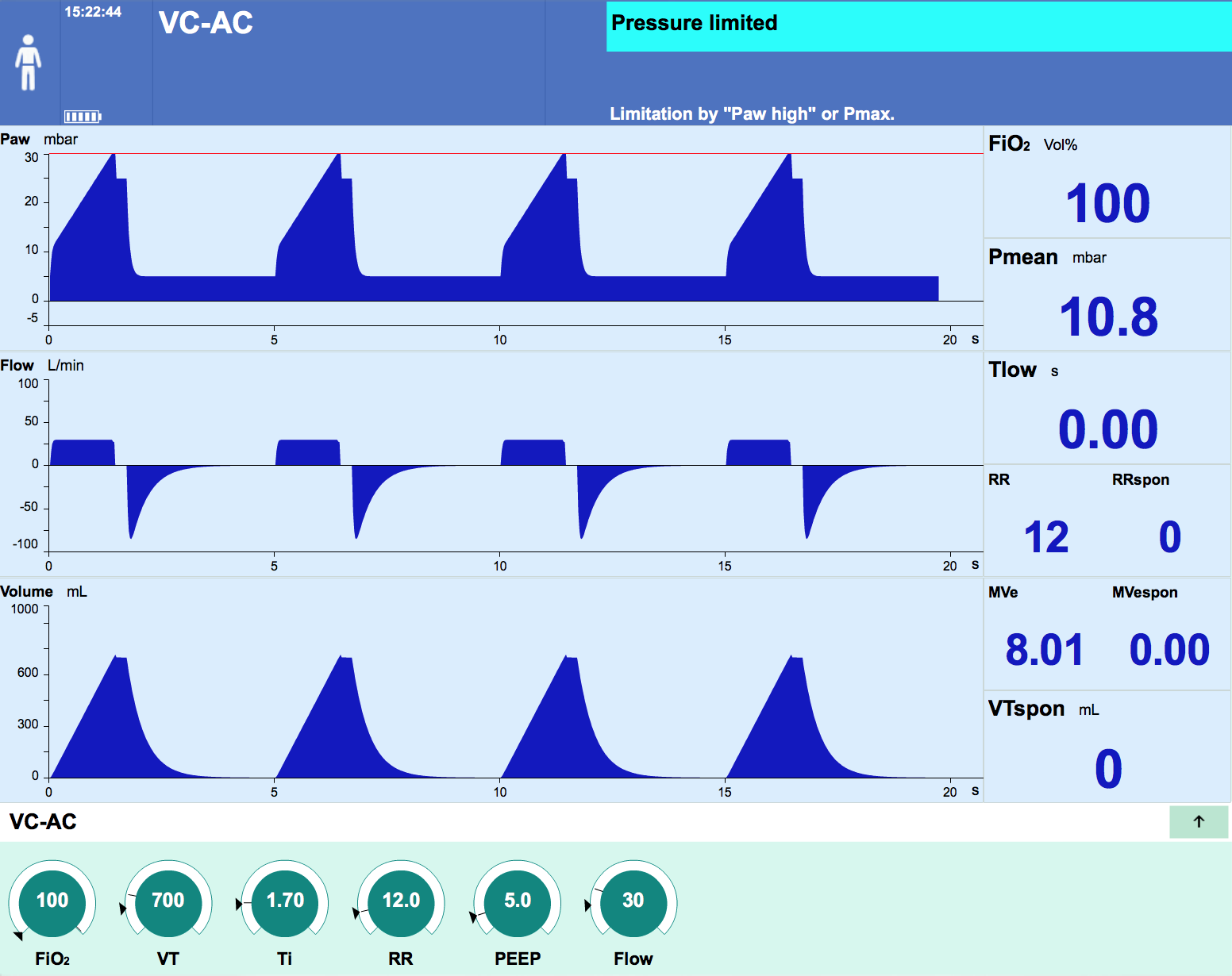
Increasing inspiratory pressures should only be required when it is is felt that the patient is hypoxic because of hypoventation. This is uncommon if the ventilator has been set appropriately.
More commonly, inspiratory pressures and tidal volumes require manipulation for CO2 clearance rather than hypoxia.
Increases to inspiratory pressures and tidal volumes must be done carefully, as this has the potential to induce barotrauma and lung injury.
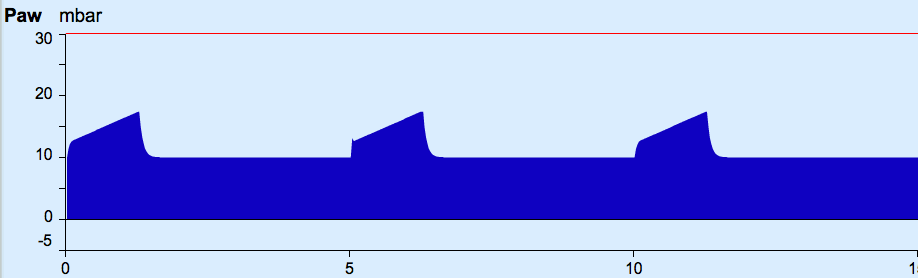
- Proportionally increases the amount of time at higher pressure
- Increases the mean pressure without increasing the peak pressure
- Potential issues:
- Alters the I:E ratio (shorter expiration) which may result in gas trapping
- May be uncomfortable for an alert patient
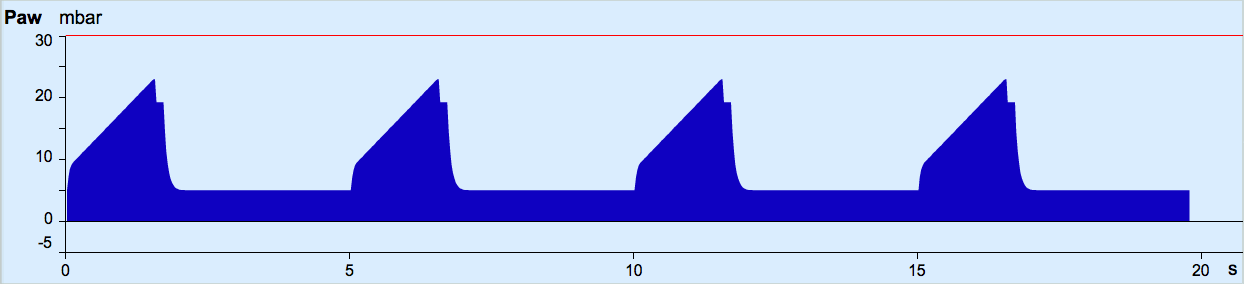
CO2 elimination
You conclude that he has acute respiratory acidosis.
Walk through the break-down tree to figure out how!
Elimination
You may recall our discussion of dead space with regard to the ventilator circuit earlier.
- Dead space is the volume of gas in each breath that does not take part in gas exchange
- Physiologic or total dead space = anatomical dead space + alveolar dead space
- Anatomical dead space is the gas within the trachea, bronchus, bronchioles and terminal bronchioles
- In normal adults it is approximately 150mL
- Alveolar dead space is the amount of gas in alveoli that are not being perfused
- Occurs in PE, pulmonary haemorrhage and hypotension
- Anatomical dead space is the gas within the trachea, bronchus, bronchioles and terminal bronchioles
- Circuit dead space contributes to anatomical dead space in ventilated patients
- This includes anything beyond the Y connector in the circuit: gas in ETT, catheter mounts, HMEs and closed suction systems
- This can become significant in paediatric patients or patients with low tidal volumes

 PEEP
PEEP dead space
dead space