Clinical Case
The ventilator is now ready to be used and may be connected to your patient. We know it will deliver breaths to your patient, but there are a few more intricacies. Let’s explore some basic ventilation physics to help you better understand your patient and subsequently adjust your ventilator settings.
Mechanical Ventilation
The ventilator has 2 main roles:
- To deliver gas into the patient as inspiration, to provide oxygenation
- To allow the passive outflow of gas during expiration and facilitate carbon dioxide clearance
To explore the physics involved in this process, the lung-ventilator unit can be represented by a tube and balloon, as illustrated below
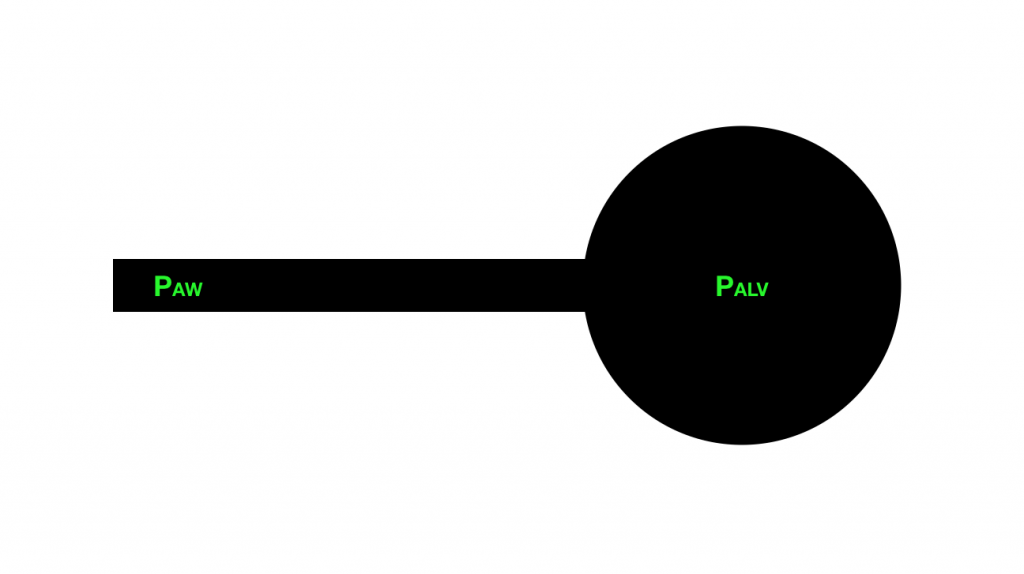
Tube = ventilator tubing + ETT + major airways
Balloon = lung alveoli
PAW = Airway pressure (what the ventilator can measure)
PALV = Alveolar pressure (what the alveoli really feel)
Pulmonary Compliance
Pulmonary compliance refers to the ease with which the lungs and thoracic cage expand for a given pressure delivered by the ventilator. It is dependent on the elasticity of the tissues involved.
Compliance = ∆V/∆P (mL/cmH2O)
In mechanically ventilated patients with normal lungs, the respiratory system’s compliance is 50-100 mL/cmH2O.
In order to deliver a volume of breath, ∆P is the pressure needed to overcome the elastic recoil of the lung and chest wall. This pressure change required to drive a change in volume is the system elastance, and is the reciprocal of compliance.
Calculate your patient’s compliance if they achieve a tidal volume of 500mL with a driving pressure of 14cmH2O.
Pulmonary Resistance
Resistance refers to the impedance of flow. Clinically, resistance is the opposition to gas flow within a respiratory unit.
Resistance = ∆P/flow (cmH2O/L/s)
Hence, this ∆P is the pressure needed to overcome the resistance of the ETT and airways to be able to generate flow of gas. It is called the Resistive Pressure (PResist) and is directly proportional to the resistance of the system.
In intubated and mechanically ventilated patients with normal lungs, the resistance is 1-8 cmH2O/L/s.
Calculate your patient’s pulmonary resistance if 4.5cmH2O of pressure is required to generate a flow of 20L/min
Overview of Inflating Pressures
To inflate the lung-ventilator unit pressure is required to both overcome the resistance in the tube that opposes gas flow and to distend the balloon where:
- Pressure required to overcome the resistance in the tube is determined by the flow down the tube and the resistance to flow
- PResist = Flow x Resistance
- Pressure required to distend the balloon (alveolar inflation pressure) is determined by the volume of gas passing into the balloon and the compliance of the balloon
- PElast = Volume / Compliance
- Therefore, the total pressure required to inflate the balloon is:
- PTOT = PResist+ PElast
- = (Flow x Resistance) + (Volume/Compliance)
The airway pressure (or PAW) is the sum of all pressures within the respiratory unit. This is what the ventilator measures.
Includes both the pressure required to inflate the alveoli (PTOT) and the baseline pressure in the balloon. As discussed, this baseline pressure is the selected PEEP
-
- So…
- PAW = PResist + PElast + PEEP
- or
- PAW = (Flow x Resistance) + (Volume/Compliance) + PEEP
Airway vs Alveolar Pressure
Lets review some of the important differences between these pressures again.
PAW = PResist + Pelast + PEEP
PAW = (Flow x Resistance) + (Volume/Compliance) + PEEP
- While alterations in flow or resistance will affect the PAW, they will not necessarily reflect alterations in the alveolar pressure (Pelast). For example, high airway pressure with bronchospasm is due to resistance in the airways (flow/resistance) rather than increased alveolar pressure. PAW is monitored routinely on the ventilator as Peak Inspiratory Pressure (PIP). The first curve displayed on your ventilator screen is usually PAW over time:
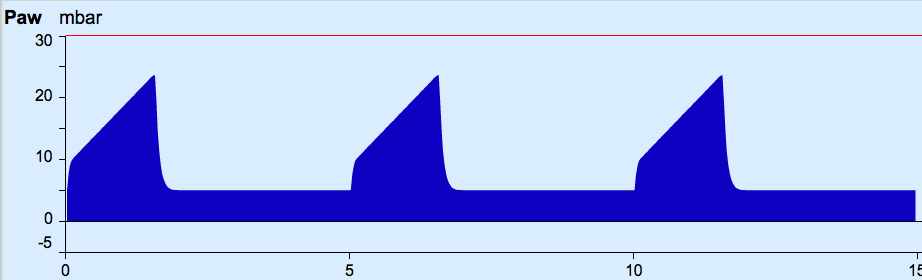
The maximum acceptable is PIP usually < 35cmH2O, but this doesn’t necessarily tell us what the alveolar pressure is…
PALV = (Volume/Compliance) + PEEP
In order to measure the Alveolar pressure, we need to measure PAW when flow is reduced to zero, so that
PAW = (0 x Resistance) + (Volume/Compliance) + PEEP
Such that
PAW = 0 + (Volume/Compliance) + PEEP
Or
PAW = PALV
To achieve a state of no flow, alveolar pressure is measured using an inspiratory pause. This is also known as the plateau pressure (Pplat).
Usually, an inspiratory hold requires the patient to be paralysed and to be on a volume controlled mode. The resulting measure is called a plateau pressure (Pplat) and is in fact the alveolar pressure.
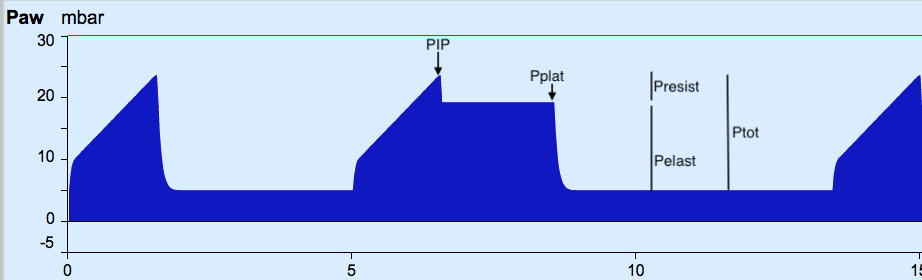
PALV should be kept < 30cmH2O to minimise lung injury
You are curious to see what your patient’s Pplat is so you proceed to an inspiratory hold. The results are: PIP 24cmH2O, Pplat 19cmH2O.
So, you had set a tidal volume (TV) of 500mL, flow at 20L/min and PEEP at 5cmH2O; the PIP is 24cmH2O, and the Pplat 19cmH2O… Can you calculate the compliance and resistance of your patient again?
